Speak directly to the analyst to clarify any post sales queries you may have.
A concise and actionable orientation to the current substance abuse treatment landscape, synthesizing clinical, technological, and policy drivers that demand executive attention
The landscape of substance abuse treatment is evolving rapidly as clinical practice, technology, and public policy converge to reshape care delivery. This executive summary synthesizes recent developments that matter most to leaders across payers, providers, and product innovators, highlighting where operational priorities and patient needs intersect. It emphasizes practical implications for treatment modalities, provider networks, and payer arrangements while clarifying how demographic change and care preferences drive demand.Moving from observation to application, the narrative connects emerging evidence with decision-focused insight. It delineates how shifts in clinical protocols, digital therapeutics, and care coordination are creating new pathways for engagement across diverse populations. The goal is to equip executives with a distillation of complex trends so they can prioritize investments, refine service models, and align governance with evolving regulatory expectations. By articulating immediate pressures and medium-term structural changes, the introduction frames the deeper analysis that follows and positions leaders to act decisively in a sector where timely adaptation is critical
How clinical innovation, telehealth adoption, and payment reforms are collectively redefining care delivery models and operational imperatives in substance abuse treatment
Care delivery for substance use disorders is undergoing transformative shifts driven by clinical innovation, digital expansion, and policy reform. Integrated care models are gaining traction as behavioral health is increasingly embedded within primary care settings and hospital systems, enabling earlier identification and streamlined referral paths. At the same time, telehealth has moved from a contingency solution to a core modality, expanding access while introducing new considerations around continuity of care, licensure, and digital equity.Value-based payment discussions are prompting providers to develop longitudinal treatment pathways that emphasize sustained recovery and outcomes measurement. Concurrently, advances in medication-assisted treatment protocols and harm reduction strategies are altering clinical workflows and reshaping community partnerships. The workforce is also adapting; clinicians and peer support specialists are adopting hybrid roles that combine in-person engagement with remote monitoring and outreach. As a result, operational design must prioritize interoperability, workforce development, and care coordination to capitalize on these structural shifts and translate them into measurable improvements in patient retention and recovery
Assessing the downstream effects of 2025 tariff adjustments on supply chains, technology procurement, and operational cost structures across treatment providers
The policy environment surrounding trade and tariffs can have indirect but meaningful effects on the substance abuse treatment sector through supply chains, pharmaceutical inputs, and technology procurement. Tariff adjustments implemented in 2025 that affect imported medical supplies, electronic hardware, and select pharmaceutical components can increase acquisition costs for treatment providers that rely on global vendors. These cost pressures may be felt most acutely by hospital-based centers and standalone facilities that maintain inventory of medical detox equipment, monitoring devices, and telehealth peripherals.Moreover, higher import duties can incentivize diversification of suppliers and accelerated procurement of domestic alternatives, prompting longer-term shifts in vendor relationships and contracting strategies. For technology-driven services, tariffs on communication equipment and patient monitoring hardware may slow the deployment cadence for synchronous telehealth solutions and remote monitoring kits. In response, payers and providers will likely prioritize inventory optimization, bulk purchasing agreements, and greater use of software-centric interventions that reduce dependence on tariff-exposed hardware.
Transitioning procurement strategies toward resilience will require closer collaboration between supply chain managers, clinical leaders, and finance teams to reconcile care quality with cost containment. Policy-driven price pressure also elevates the strategic importance of local manufacturing, pooled purchasing arrangements, and total cost of care analyses that capture the downstream implications of tariff-induced input cost changes. Ultimately, stakeholders who proactively adjust sourcing, contracting, and care delivery plans will be better positioned to sustain service continuity and preserve patient access
A segmentation-driven framework that links treatment modes, substance types, provider settings, end-user cohorts, and payment mechanisms to operational and clinical decision-making
Understanding segmentation is essential to designing services that reflect clinical needs, payer expectations, and patient preferences across multiple care pathways. When treatment modes are examined, day treatment, detoxification, inpatient, outpatient, and telehealth each reveal distinct operational footprints; detoxification divides into medical and non-medical approaches with separate staffing and monitoring requirements, inpatient care splits between hospital-based and residential settings that vary in intensity and regulatory oversight, outpatient services range from intensive outpatient programs to standard outpatient models with differing session cadences, and telehealth encompasses both asynchronous and synchronous modalities that influence triage, engagement, and follow-up.Substance type further frames clinical protocols and resource allocation because alcohol, cannabis, opioids, and stimulants present unique pharmacologic and psychosocial management needs that shape therapeutic pathways. Provider type matters as clinics, homecare teams, hospital-based centers, and standalone rehabilitation facilities carry distinct capital, workforce, and licensing profiles that affect scalability and care continuity. End users-adolescents, adults, and geriatric populations-require age-appropriate engagement strategies, family involvement considerations, and comorbidity management approaches tailored to each cohort.
Payment mode is a foundational determinant of access and sustainability; private insurance, public funding, and self-pay models create divergent revenue dynamics and compliance obligations that influence program design and patient navigation. Integrating these segment lenses reveals where clinical innovation, reimbursement strategy, and operational design must align to support retention, outcomes measurement, and equitable access. By translating segmentation into actionable program differentiation, leaders can prioritize investments that match clinical complexity with provider capacity and payer incentives
How regional regulatory environments, cultural drivers, and payer structures in the Americas, Europe Middle East & Africa, and Asia-Pacific shape tailored strategies for treatment delivery
Regional context shapes how services are delivered, reimbursed, and regulated, which in turn informs strategic choices about network design and resource allocation. In the Americas, policy emphasis on expanding access and integrating behavioral health into primary care has driven growth in outpatient and telehealth capacities, while diverse payer mixes create both opportunity and complexity for reimbursement negotiations. In contrast, Europe, Middle East & Africa present a heterogeneous regulatory landscape where cross-border workforce mobility, variable funding mechanisms, and differing public health priorities require adaptive program models and strong local partnerships.Asia-Pacific markets are characterized by rapid digital health adoption, varying degrees of stigma-driven underutilization, and significant urban-rural disparities in provider availability. Each region therefore demands tailored approaches to workforce training, digital inclusion, and community engagement. Transitional strategies that account for regional payer structures and cultural drivers will enhance adoption of best practices and support scalable models. Moreover, regional collaboration on knowledge exchange and capacity building can accelerate the diffusion of effective care models while respecting local governance and funding constraints. Ultimately, a regionally nuanced strategy enables more precise alignment between service offerings and the regulatory, cultural, and payer realities that shape patient access
An overview of how providers, technology innovators, pharmaceutical suppliers, and payers are aligning around integrated care, digital tools, and outcome-oriented arrangements
Key companies operating in the substance abuse treatment ecosystem span clinical service providers, technology vendors, pharmaceutical manufacturers, and payers that fund care pathways. Clinical organizations are differentiating through integrated care models, telehealth-enabled continuity, and partnerships that extend behavioral health expertise into primary care and community settings. Technology vendors are advancing solutions for remote monitoring, digital therapeutics, and care coordination platforms that streamline clinician workflows and support patient engagement across treatment episodes.Pharmaceutical companies continue to focus on evidence generation for medication-assisted therapies and on ensuring supply chain continuity for essential compounds. Payers and managed care entities are increasingly incorporating performance metrics and outcome-based arrangements that incentivize sustained recovery and reduce avoidable acute care utilization. Strategic alliances between these stakeholder groups are emerging to pilot bundled payment models, shared care registries, and data interoperability initiatives that emphasize measurable outcomes. Organizations that combine clinical depth with scalable technology and payer-aligned metrics are establishing competitive advantage by delivering higher-value care while managing cost and compliance obligations
Practical and prioritized actions for executives to build procurement resilience, digital interoperability, payer alignment, workforce capacity, and outcome-focused care models
Industry leaders should pursue a set of pragmatic actions that balance short-term operational resilience with long-term transformation. First, strengthen procurement and supply chain strategies to reduce exposure to external shocks by diversifying vendors, negotiating longer-term contracts, and assessing opportunities for domestic sourcing where appropriate. Second, invest in interoperable digital platforms that support both asynchronous and synchronous care, and ensure that these platforms are integrated with electronic health records to maintain continuity and data integrity.Third, align clinical pathways with payment models by collaborating with payers on outcome definitions, measurement frameworks, and pilot arrangements that reward sustained recovery. Fourth, prioritize workforce development through targeted upskilling of clinicians and peer staff in remote engagement techniques, trauma-informed care, and measurement-based treatment. Fifth, design age- and substance-specific programming that reflects the needs of adolescents, adults, and geriatric patients while embedding family and community supports where relevant.
Finally, adopt a phased approach to innovation that pairs rigorous evaluation with rapid-cycle iteration so organizations can scale what works and discontinue what does not. Together, these steps create a resilient foundation for improving clinical outcomes, enhancing access, and sustaining financial viability in a complex operating environment
A transparent, multi-source research methodology combining clinical literature, regulatory reviews, interviews, and operational analysis to produce actionable insights for stakeholders
The research underpinning this analysis synthesizes peer-reviewed clinical literature, regulatory guidance, industry technical standards, and primary interviews with clinical leaders, payer executives, and digital health innovators. Data triangulation ensured that operational observations were corroborated across multiple sources and perspectives, and that thematic conclusions reflected both frontline practice and strategic planning horizons. The methodology placed particular emphasis on care pathway mapping, segment alignment, and the operational implications of policy and procurement shifts.Qualitative inputs from practitioners were combined with regulatory reviews and vendor capability assessments to identify practical levers for implementation. Where relevant, comparative regional analysis highlighted how governance and funding differences influence adoption and scale. The approach balanced depth and breadth to provide insight that is both actionable at the organizational level and relevant for system-wide strategy discussions. Transparency in sources and methodological choices supports reproducibility and allows stakeholders to tailor follow-up inquiries to their specific decision needs
Concluding synthesis that emphasizes patient-centered care, interoperable technology, procurement resilience, and collaborative payer-provider partnerships as priorities for sustained progress
The cumulative analysis demonstrates that substance abuse treatment is at an inflection point where clinical advances, technology diffusion, and policy realignment converge to create both opportunity and operational complexity. Providers who adopt interoperable platforms, diversify supply chains, and align clinical pathways with payer incentives are better positioned to deliver sustained outcomes. Regions and provider types will require tailored approaches, but common principles-patient-centered care, measurement-based pathways, and resilient procurement-apply broadly.Decision-makers must balance the imperative to expand access with the need to maintain care quality and financial sustainability. That balance will be achieved through disciplined program design, targeted workforce investment, and strategic partnerships that link clinical capacity with reimbursement innovation. By embracing iterative evaluation and close collaboration across stakeholders, organizations can transform emerging pressures into a strategic advantage and deliver measurable improvements in recovery and population health
Additional Product Information:
- Purchase of this report includes 1 year online access with quarterly updates.
- This report can be updated on request. Please contact our Customer Experience team using the Ask a Question widget on our website.
Table of Contents
7. Cumulative Impact of Artificial Intelligence 2025
17. China Substance Abuse Treatment Market
Companies Mentioned
The key companies profiled in this Substance Abuse Treatment market report include:- Acadia Healthcare Company, Inc.
- Advanced Recovery Systems, LLC
- American Addiction Centers, Inc.
- Caron Treatment Centers, Inc.
- CleanSlate Centers, LLC
- Hazelden Betty Ford Foundation
- Odyssey House, Inc.
- Orexo AB
- Phoenix House Foundation
- Recovery Centers of America, LLC
- Universal Health Services, Inc.
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 183 |
| Published | January 2026 |
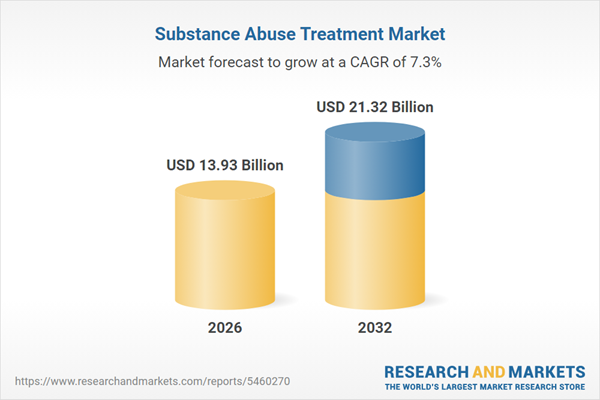
| Forecast Period | 2026 - 2032 |
| Estimated Market Value ( USD | $ 13.93 Billion |
| Forecasted Market Value ( USD | $ 21.32 Billion |
| Compound Annual Growth Rate | 7.2% |
| Regions Covered | Global |
| No. of Companies Mentioned | 12 |