High adoption of digital technologies such as electronic health records, revenue cycle management software, mhealth applications, telehealth, and increasing efforts towards digitalization of healthcare in the U.S. are positively driving the growth of the U.S. medical coding industry. In 2021, about 88.2% of physicians' offices were using electronic health records in the U.S., as per data provided by the Centers for Disease Control and Prevention.
Moreover, increasing utilization of medical coding in the revenue cycle management process includes new revisions in codes to increase flexibility and scalability. The new ICD-11 was implemented in January 2022, including several new chapters that support electronic health records. It has approximately 55 thousand codes for the classification of disorders, diseases, injuries, and deaths. Moreover, many new codes were created during the COVID-19 pandemic for COVID-19 and telehealth. The World Health Organization introduced new ICD-10 codes, which came into effect between April and September 2020. Thus, the introduction and revisions of codes are positively impacting market growth
The Bureau of Labor Statistics, Office of Occupational Statistics and Employment Projections, estimated that the number of employees in medical records and health information is estimated to grow by 7% between 2021 and 2031. Certified medical coders are one of the most sought-after jobs in the U.S. Increasing demand for a universal language in medical documentation positively impacts the demand for medical coders and the coding industry.
The increasing workload on healthcare staff and physicians for medical coding is increasing the adoption of various automation solutions. For instance, according to a survey conducted by Athenahealth, physicians are working overtime for an average of 90 minutes for coding. There is an increase in the adoption of computer-assisted coding solutions for rapid, accurate, and efficient medical coding. Computer-assisted coding can increase productivity by 11-30%, as per a survey conducted by 3M.
Furthermore, the development of artificial intelligence (AI)-enabled medical coding is estimated to drive market growth. For instance, in August 2025, HGM Limited, through its U.S. subsidiary Healthcare Capital Holdings LLC (HCH), announced the acquisition of Aidéo Technologies LLC, a leader in AI-powered autonomous coding solutions. This acquisition expands HGM’s capabilities in revenue cycle management (RCM), medical coding, and healthcare analytics.
“Acquiring Aidéo Technologies is a major step towards our goal of building a comprehensive AI-driven healthcare services platform. Aidéo’s Autonomous Coding Platform, built on advanced AI, natural language processing, real-time analytics, and Large Language Models (LLM), delivers accuracy that surpasses manual and traditional CAC tools. Its HL7 interoperability ensures seamless communication with industry standard EHR systems, supporting surgical specialties, emergency departments, anesthesia, radiology, and RCM companies across the U.S.”
- Dr. Bhargav Thakkar, EVP Healthcare of HGM Limited.
U.S. Medical Coding Market Report Segmentation
This report forecasts revenue growth at the country level and provides an analysis of the latest industry trends in each of the sub-segments from 2021 to 2033. The analyst has segmented the U.S. medical coding market report based on classification system, component, and medical specialty:Classification System Outlook (Revenue, USD Million, 2021-2033)
- ICD
- HCPCS
- CPT
Component Outlook (Revenue, USD Million, 2021-2033)
- In-house
- Outsourced
- Onshore
- Offshore
Medical Specialty Outlook (Revenue, USD Million, 2021-2033)
- Oncology
- Cardiology
- Anesthesia
- Radiology
- Pathology
- Pain Management
- Emergency Services
- Others
Why should you buy this report?
- Comprehensive Market Analysis: Gain detailed insights into the industry across major regions and segments.
- Competitive Landscape: Explore the market presence of key players.
- Future Trends: Discover the pivotal trends and drivers shaping the future of the market.
- Actionable Recommendations: Utilize insights to uncover new revenue streams and guide strategic business decisions.
This report addresses:
- Market intelligence to enable effective decision-making
- Market estimates and forecasts from 2018 to 2030
- Growth opportunities and trend analyses
- Segmental and regional revenue forecasts for market assessment
- Competition strategy and market share analysis
- Product innovation listings for you to stay ahead of the curve
- COVID-19's impact and how to sustain in these fast-evolving markets
This product will be delivered within 1-3 business days.
Table of Contents
Companies Mentioned
The major companies profiled in this U.S. Medical Coding market report include:- STARTEK
- Oracle
- Maxim Healthcare Services
- Parexel International Corporation
- Aviacode Inc.
- Precyse Solutions, LLC
- Verisk Analytics, Inc.
- Medical Record Associates, LLC.
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 90 |
| Published | August 2025 |
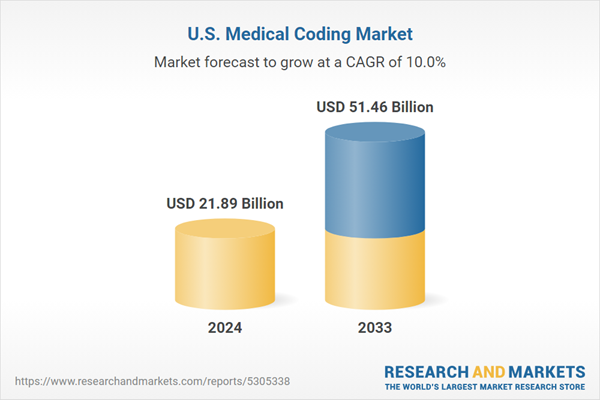
| Forecast Period | 2024 - 2033 |
| Estimated Market Value ( USD | $ 21.89 Billion |
| Forecasted Market Value ( USD | $ 51.46 Billion |
| Compound Annual Growth Rate | 10.0% |
| Regions Covered | United States |
| No. of Companies Mentioned | 9 |