Healthcare claims management is a crucial aspect of the healthcare industry that involves the process of handling and processing medical claims made by patients and healthcare providers. It encompasses the entire lifecycle of a claim, from submission to reimbursement. The primary goal of claims management is to ensure accuracy, efficiency, and timely processing of claims, while minimizing errors and maximizing revenue for healthcare organizations. At the core of healthcare claims management is the interaction between healthcare providers, insurance companies, and patients.
When a patient receives medical services, the healthcare provider submits a claim to the patient's insurance company, detailing the services rendered and requesting reimbursement. The insurance company then reviews the claim for completeness, accuracy, and compliance with its policies. This involves verifying the patient's eligibility, the appropriateness of the services provided, and the contractual obligations between the provider and the insurance company. Claims management involves various tasks, including data entry, coding, billing, claims submission, follow-up on outstanding claims, denial management, and appeals. Efficient claims management requires a deep understanding of medical coding systems, insurance policies, billing regulations, and industry standards.
The increasing complexity of healthcare billing and coding regulations necessitates claims management systems, which is creating a positive market outlook. As regulations evolve, healthcare providers must ensure accurate and compliant claims submission to avoid penalties and payment denials. This is escalating the demand for sophisticated claims management solutions that can handle the intricacies of coding, documentation, and billing requirements. Additionally, the rise in healthcare costs and the need for cost containment is propelling the market growth. Besides this, efficient claims management practices help identify and reduce billing errors, fraud, and abuse, leading to cost savings for healthcare organizations and payers.
Other than this, the shift toward value-based care models emphasizes the importance of healthcare claims management. Providers are increasingly incentivized based on outcomes and quality of care, requiring meticulous claims management to track and measure performance metrics. Furthermore, advancements in technology, such as electronic health records (EHR) and health information exchange (HIE) systems, enable seamless data exchange, improving the accuracy and speed of claims processing. Automation and artificial intelligence (AI) are also revolutionizing claims management, streamlining processes, reducing errors, and optimizing reimbursement.
Healthcare Claims Management Market Trends/Drivers:
Increasing complexity of healthcare billing and coding regulations
As regulations become more intricate and stringent, healthcare providers must navigate complex coding systems, documentation requirements, and billing guidelines to ensure accurate claims submission. Failure to comply with these regulations can result in payment denials, audits, and penalties. To address this challenge, claims management systems and processes are designed to ensure adherence to billing and coding regulations, minimize errors, and maximize reimbursement. Robust claims management solutions provide the necessary tools and expertise to navigate the evolving regulatory landscape, ensuring compliance and optimizing revenue for healthcare organizations.Rise in healthcare costs and the need for cost containment
With the increasing healthcare expenses, healthcare organizations and payers are under pressure to reduce costs and improve financial performance. Healthcare claims management plays a crucial role in identifying billing errors, fraudulent activities, and improper payments, which can contribute to unnecessary expenditures. By implementing robust claims management processes, organizations can identify and rectify these issues, leading to cost savings and improved revenue. Additionally, efficient claims management helps minimize payment delays and denials, ensuring timely reimbursement and financial stability for healthcare providers. As a result, it is a key strategy in containing costs and optimizing financial outcomes in the healthcare industry.Advancements in technology
The adoption of electronic health records (EHR) and health information exchange (HIE) systems enable seamless sharing and processing of patient data, thus enhancing the accuracy and speed of claims management. Apart from this, technological advancements empower healthcare organizations to leverage data and automation, resulting in streamlined claims management processes, improved accuracy, and enhanced revenue cycle management.Automation and artificial intelligence (AI) tools streamline claims processes, reduce manual errors and improve efficiency. Machine learning algorithms can identify patterns in claims data, detecting potential fraud or errors. Additionally, technology-driven solutions facilitate real-time eligibility verification, electronic claim submission, and electronic remittance advice, simplifying the claims management workflow.
Healthcare Claims Management Industry Segmentation:
The research provides an analysis of the key trends in each segment of the global healthcare claims management market report, along with forecasts at the global, regional, and country levels from 2025-2033. Our report has categorized the market based on the product, component, solution type, delivery mode, and end user.Breakup by Product:
- Medical Billing
- Professional
- Institutional
- Claims Processin.
Medical billing dominates the market
The report has provided a detailed breakup and analysis of the healthcare claims management market based on the product. This includes medical billing (professional and institutional) and claims processing. According to the report, medical billing accounted for the largest share.Medical billing involves the process of accurately translating medical procedures, diagnoses, and services into billing codes for reimbursement. Efficient medical billing ensures timely claims submission, reduces billing errors, and maximizes revenue for healthcare providers. By streamlining the billing process, healthcare organizations can optimize their revenue cycle, minimize payment delays, and enhance financial performance. Effective medical billing systems and practices are essential for a smooth claims management process, ensuring accurate reimbursement and financial viability for healthcare providers.
Claims processing involves the review, adjudication, and payment of submitted medical claims. Efficient claims processing ensures that claims are evaluated accurately, in compliance with payer policies and regulations. It involves tasks such as verification of patient eligibility, coding review, claims submission, and payment reconciliation. Streamlining the claims processing workflow minimizes delays, reduces errors, and enhances the overall efficiency of the claims management process. By ensuring timely and accurate claims processing, healthcare organizations can optimize revenue, improve provider-payer relationships, and enhance the overall financial health of the healthcare ecosystem.
Breakup by Component:
- Services
- Softwar.
Software holds the majority of the overall market share
A detailed breakup and analysis of the healthcare claims management market based on the component has also been provided in the report. This includes services and software. According to the report, software represented the largest market segment.Healthcare claims management software provides a digital platform to streamline the entire claims lifecycle. These solutions automate manual processes, facilitate electronic claims submission, offer coding and billing guidance, provide real-time eligibility verification, and generate analytics and reports for performance evaluation. Healthcare claims management software enhances efficiency, accuracy, and compliance, leading to improved revenue cycle management and financial outcomes for healthcare organizations. It enables seamless integration with electronic health records (EHR) systems, enhances interoperability, and promotes data-driven decision-making in the claims management process.
Healthcare claims management services offer comprehensive solutions for coding, billing, claims submission, denial management, and revenue cycle optimization. These services help healthcare providers navigate complex billing regulations, improve accuracy, reduce errors, and optimize reimbursement. By outsourcing claims management to experienced service providers, healthcare organizations can focus on delivering quality care while ensuring efficient and effective claims processing.
Breakup by Solution Type:
- Integrated Solutions
- Standalone Solution.
Integrated solutions represent the most popular solution type
The report has provided a detailed breakup and analysis of the healthcare claims management market based on the solution type. This includes integrated and standalone solutions. According to the report, integrated solutions accounted for the largest share.Integrated solutions offer comprehensive platforms that combine multiple functionalities within a single system. These solutions integrate with electronic health record (EHR) systems, billing software, and other healthcare applications, allowing seamless data exchange and streamlined workflows. Integrated solutions also provide end-to-end claims management capabilities, from coding and documentation to claims submission and payment reconciliation. They offer a unified view of patient information, automate processes, enhance accuracy, and improve efficiency. By eliminating the need for multiple disconnected systems, integrated solutions simplify the claims management process, enhance collaboration between stakeholders, and optimize revenue cycle management.
Standalone solutions offer specialized tools focused solely on claims processing and management. These solutions may provide specific functionalities like claims submission, denial management, or analytics. Standalone solutions are designed to address specific pain points to cater to specific needs of healthcare organizations. They offer targeted features and customization options, allowing organizations to choose and implement specific modules as per their requirements. Standalone solutions are flexible, scalable, and often interoperable with existing systems. They enable healthcare organizations to address specific claims management challenges efficiently, enhance productivity, and improve financial performance by addressing specific pain points.
Breakup by Delivery Mode:
- On-premises
- Cloud-based
- Web-base.
Web-based delivery mode accounts for the largest market share
The report has provided a detailed breakup and analysis of the healthcare claims management market based on the delivery mode. This includes on-premises, cloud-based, and web-based. According to the report, web-based accounted for the largest share.Web-based delivery mode of healthcare claims management is the process of handling and processing medical claims using online platforms or web-based systems. Healthcare providers submit claims electronically through web portals or dedicated software systems. These claims contain information such as patient details, services rendered, diagnosis codes, and associated costs. It involves the submission, processing, adjudication, and payment of claims for medical services provided to patients. Web-based systems can access real-time eligibility data to determine if a patient is covered by insurance and if the services provided are eligible for reimbursement.
Moreover, web portals allow for secure and direct communication between healthcare providers and payers, thereby facilitating quicker resolution of claim-related inquiries and issues.On-premises delivery mode allows organizations to host and manage their claims management systems internally. This mode provides complete control over the infrastructure, data security, and customization options. On-premises solutions are preferred by organizations with specific security and compliance requirements, allowing them to maintain sensitive patient data within their own premises.
Cloud-based delivery mode drives the claims management market by providing web-based solutions hosted on remote servers. Cloud-based solutions offer flexibility, scalability, and accessibility from anywhere with an internet connection. They eliminate the need for complex on-site infrastructure, reduce maintenance costs, and provide automatic software updates. Cloud-based solutions enable rapid deployment, easy integration, and seamless data sharing, promoting collaboration between stakeholders and enabling efficient claims management across multiple locations and devices.
Breakup by End User:
- Healthcare Payers
- Healthcare Providers
- Others
Healthcare payers drive the claims management process by setting policies, guidelines, and reimbursement rates for healthcare services. They establish the rules and requirements that healthcare providers must follow when submitting claims for reimbursement. Payers play a crucial role in evaluating and adjudicating claims, ensuring compliance with regulatory standards, and managing payment processes. They invest in advanced claims management systems, employ skilled professionals, and implement fraud detection mechanisms to optimize claims processing and cost containment.
Healthcare providers drive claims management by submitting accurate and complete claims for reimbursement to payers. They are responsible for coding medical services, documenting patient encounters, and submitting claims in a timely manner. Providers invest in efficient claims management processes, software, and staff training to minimize errors, avoid claim denials, and maximize reimbursement. They also collaborate with payers to understand and adhere to the evolving reimbursement policies, ensure proper documentation, and engage in appeals and follow-ups for denied claims. Providers continuously strive to improve claims management efficiency to optimize revenue and financial sustainability.
Breakup by Region:
- North America
- United States
- Canada
- Asia-Pacific
- China
- Japan
- India
- South Korea
- Australia
- Indonesia
- Others
- Europe
- Germany
- France
- United Kingdom
- Italy
- Spain
- Russia
- Others
- Latin America
- Brazil
- Mexico
- Others
- Middle East and Afric.
North America exhibits a clear dominance, accounting for the largest healthcare claims management market share
The report has also provided a comprehensive analysis of all the major regional markets, which include North America (the United States and Canada); Europe (Germany, France, the United Kingdom, Italy, Spain, Russia, and others); Asia Pacific (China, Japan, India, South Korea, Australia, Indonesia, and others); Latin America (Brazil, Mexico, and others); and the Middle East and Africa. According to the report, North America was the largest market for healthcare claims management.In North America, there has been a growing adoption of claims management in the healthcare sector due to robust healthcare infrastructure, stringent regulatory environment, and technological advancements. The region emphasizes on efficient claims processing, fraud detection, and cost containment. It invests in innovative claims management solutions, leverages electronic health records (EHR) integration, and adopts advanced analytics to optimize revenue cycles and improve patient outcomes.
Europe healthcare claims management focuses on interoperability, standardized coding systems, and cost-effective healthcare delivery. The region emphasizes value-based care models, patient-centric approaches, and cross-border cooperation for seamless claims processing and reimbursement. It invests in integrated health information systems, data sharing platforms, and telemedicine solutions to streamline claims management processes and enhance overall healthcare efficiency.
The rapid digital transformation, expanding healthcare access, and growing health insurance is driving the Asia Pacific healthcare claims management market. The region leverages technological advancements, such as cloud computing and mobile health solutions, to improve claims processing and reimbursement accuracy. It emphasizes scalability, affordability, and interoperability of claims management systems to cater to diverse healthcare settings and populations. Asia Pacific also focuses on innovative payment models, regulatory reforms, and adoption of electronic claim submission to drive efficient claims management and financial sustainability in the healthcare industry.
Competitive Landscape:
The key players in the healthcare claims management market have undertaken various efforts to drive advancements and innovation in the industry. They have invested in developing robust claims management software and platforms that integrate with electronic health records (EHR) systems, enabling seamless data exchange and efficient claims processing. Additionally, these players have focused on incorporating automation and artificial intelligence (AI) technologies to streamline claims workflows, improve accuracy, and reduce manual errors. Furthermore, key players have actively collaborated with healthcare providers and payers to understand their specific needs and challenges, tailoring their solutions accordingly.They have also engaged in partnerships and acquisitions to expand their offerings and strengthen their market presence. Additionally, the leading players are emphasizing the importance of compliance with evolving regulatory requirements, ensuring their solutions meet the necessary standards. Moreover, key players have invested in research and development to continuously enhance their claims management solutions, incorporating predictive analytics, machine learning, and data-driven insights to drive process efficiency and optimize revenue cycles. These efforts collectively drive the growth and advancement of the healthcare claims management market.
The report has provided a comprehensive analysis of the competitive landscape in the global healthcare claims management market. Detailed profiles of all major companies have also been provided. Some of the key players in the market include:
- Accenture Plc
- Allscripts Healthcare Solutions Inc.
- Athenahealth
- Carecloud Inc.
- Cognizant
- Conifer Health Solutions (Tenet Healthcare Corporation)
- Mckesson Corporation
- Optum Inc. (United Health Group Incorporated)
- Oracle Corporation
- Plexis Healthcare Systems
- Quest Diagnostics
- The SSI Group LLC.
Key Questions Answered in This Report
- How big is the global healthcare claims management market?
- What is the expected growth rate of the global healthcare claims management market during 2025-2033?
- What are the key factors driving the global healthcare claims management market?
- What has been the impact of COVID-19 on the global healthcare claims management market?
- What is the breakup of the global healthcare claims management market based on the product?
- What is the breakup of the global healthcare claims management market based on the component?
- What is the breakup of the global healthcare claims management market based on the solution type?
- What is the breakup of the global healthcare claims management market based on the delivery mode?
- What are the key regions in the global healthcare claims management market?
- Who are the key players/companies in the global healthcare claims management market?
Table of Contents
Companies Mentioned
- Accenture plc
- Allscripts Healthcare Solutions Inc.
- Athenahealth
- Carecloud Inc.
- Cognizant
- Conifer Health Solutions (Tenet Healthcare Corporation)
- Mckesson Corporation
- Optum Inc. (United Health Group Incorporated)
- Oracle Corporation
- Plexis Healthcare Systems
- Quest Diagnostics
- The SSI Group LLC
Table Information
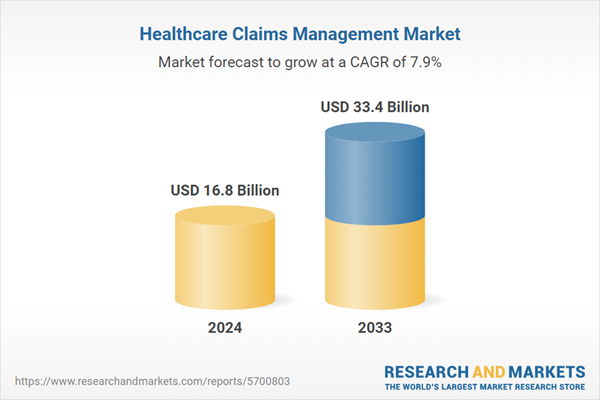
| Report Attribute | Details |
|---|---|
| No. of Pages | 135 |
| Published | June 2025 |
| Forecast Period | 2024 - 2033 |
| Estimated Market Value ( USD | $ 16.8 Billion |
| Forecasted Market Value ( USD | $ 33.4 Billion |
| Compound Annual Growth Rate | 7.9% |
| Regions Covered | Global |
| No. of Companies Mentioned | 12 |