Global Healthcare Fraud Detection Market - Key Trends & Drivers Summarized
Why Has Fraud Detection Become a Priority Across Global Healthcare Systems?
Healthcare fraud detection has become a critical pillar of operational integrity and financial sustainability for healthcare payers, providers, and governments. Fraudulent activities such as upcoding, phantom billing, kickbacks, identity theft, and prescription fraud result in billions of dollars in losses annually, straining public budgets and private insurance systems alike. The growing complexity of healthcare billing systems, combined with the digitization of health records and claims, has made it easier for fraudulent actors to exploit systemic loopholes - necessitating advanced detection tools to maintain accountability and reduce economic waste.Increased scrutiny from regulators and a surge in value-based reimbursement models are accelerating the need for real-time fraud prevention. Health systems are shifting from reactive audits to proactive surveillance using predictive analytics, machine learning, and anomaly detection. As fraud schemes evolve in sophistication, especially in digitally enabled claims environments, the emphasis is moving toward intelligent systems that detect irregularities before they result in payments, rather than relying on post-transaction investigations.
How Are Data Analytics and AI Revolutionizing Fraud Detection Capabilities?
The application of artificial intelligence (AI) and big data analytics has dramatically enhanced the capabilities of fraud detection systems. Predictive modeling algorithms can now analyze millions of claims, electronic health records (EHRs), and provider behavior patterns to identify suspicious deviations. Unsupervised learning models are particularly effective at uncovering new fraud schemes by clustering similar behavior and flagging outliers in real time. Natural language processing (NLP) is also being used to scan unstructured data sources like doctor notes and insurance correspondence to identify discrepancies and unusual billing language.Additionally, AI-based scoring systems assign fraud risk levels to claims and providers, enabling insurers and investigators to prioritize high-risk targets. Blockchain is gaining interest as a secure, immutable platform for verifying transactions and maintaining transparency across health ecosystems. Combined with robust data governance and interoperability frameworks, these technologies are improving detection accuracy, reducing false positives, and accelerating resolution timelines - all of which contribute to more cost-effective and responsive fraud management.
Which Stakeholders and Regions Are Leading Adoption of Fraud Detection Systems?
Insurance companies and public health programs are leading adopters of healthcare fraud detection technologies due to their exposure to large-scale claims processing. In the U.S., Medicare and Medicaid programs have driven innovation through large-scale anti-fraud initiatives and partnerships with data analytics firms. Private insurers are investing heavily in AI platforms to protect premium revenues and maintain regulatory compliance. Meanwhile, providers are also implementing internal fraud risk controls to avoid litigation, protect reputational capital, and comply with payer contracts.Regionally, North America holds the largest market share due to the complexity of its insurance landscape and the scale of fraudulent activity. Europe is following closely, with national health systems introducing centralized monitoring mechanisms and predictive audit tools. In Asia-Pacific and Latin America, increasing digitization of claims and healthcare infrastructure is paving the way for fraud detection platform adoption, especially as universal healthcare programs expand and private insurance markets grow. Cross-border data-sharing initiatives are also emerging to combat international fraud rings, especially in telemedicine and pharmaceutical distribution.
The Growth in the Healthcare Fraud Detection Market Is Driven by Several Factors
The growth in the healthcare fraud detection market is driven by the escalating scale and complexity of fraud schemes, rising healthcare expenditure, and increasing regulatory enforcement worldwide. The transition to digital health records and automated billing has created fertile ground for fraud but also enables robust data analytics to counteract it. The adoption of AI, machine learning, and blockchain technologies is transforming fraud detection from a retrospective audit function into a real-time, risk-based decision-making capability.Payers and providers alike are under growing pressure to reduce administrative waste, recover lost revenue, and ensure compliance with reimbursement policies and government regulations. Investments in integrated fraud detection systems are now seen as essential to operational efficiency and financial control. As healthcare ecosystems become more interconnected and data-driven, fraud detection is evolving into a foundational capability that supports trust, transparency, and sustainability in modern healthcare delivery.
Report Scope
The report analyzes the Healthcare Fraud Detection market, presented in terms of market value (US$). The analysis covers the key segments and geographic regions outlined below:- Segments: Type (Descriptive Analytics, Predictive Analytics, Prescriptive Analytics); Application (Review Of Insurance Claims, Payment Integrity); End-Use (Private Insurance Payers, Government Agencies, Other End-Uses).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; Spain; Russia; and Rest of Europe); Asia-Pacific (Australia; India; South Korea; and Rest of Asia-Pacific); Latin America (Argentina; Brazil; Mexico; and Rest of Latin America); Middle East (Iran; Israel; Saudi Arabia; United Arab Emirates; and Rest of Middle East); and Africa.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Descriptive Analytics segment, which is expected to reach US$5.4 Billion by 2030 with a CAGR of a 27.6%. The Predictive Analytics segment is also set to grow at 20.9% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $561.2 Million in 2024, and China, forecasted to grow at an impressive 33.8% CAGR to reach $2 Billion by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Healthcare Fraud Detection Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Healthcare Fraud Detection Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Healthcare Fraud Detection Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as BSA LifeStructures, CannonDesign, CPL Team, DLR Group, E4H Environments for Health and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 44 companies featured in this Healthcare Fraud Detection market report include:
- CGI Inc.
- Codoxo
- Conduent Inc.
- Cotiviti
- DXC Technology
- EXL Service Holdings Inc.
- Fair Isaac Corporation (FICO)
- HCL Technologies Ltd.
- Healthcare Fraud Shield
- IBM Corporation
- LexisNexis Risk Solutions
- McKesson Corporation
- Northrop Grumman Corporation
- Optum Inc. (UnitedHealth Group)
- OSP Labs
- RLDatix
- SAS Institute Inc.
- Shift Technology
- Verisk Analytics
- Wipro Ltd.
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- CGI Inc.
- Codoxo
- Conduent Inc.
- Cotiviti
- DXC Technology
- EXL Service Holdings Inc.
- Fair Isaac Corporation (FICO)
- HCL Technologies Ltd.
- Healthcare Fraud Shield
- IBM Corporation
- LexisNexis Risk Solutions
- McKesson Corporation
- Northrop Grumman Corporation
- Optum Inc. (UnitedHealth Group)
- OSP Labs
- RLDatix
- SAS Institute Inc.
- Shift Technology
- Verisk Analytics
- Wipro Ltd.
Table Information
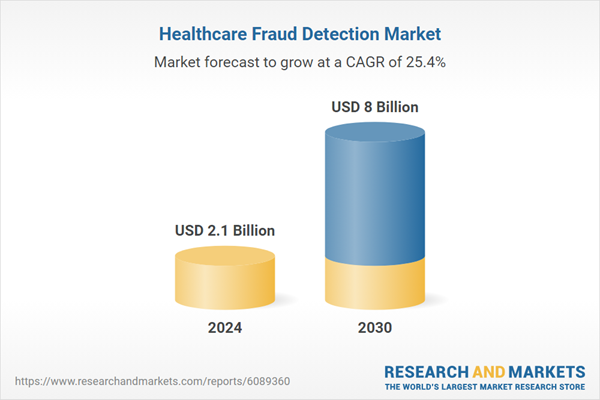
| Report Attribute | Details |
|---|---|
| No. of Pages | 374 |
| Published | February 2026 |
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 2.1 Billion |
| Forecasted Market Value ( USD | $ 8 Billion |
| Compound Annual Growth Rate | 25.4% |
| Regions Covered | Global |