Speak directly to the analyst to clarify any post sales queries you may have.
The Healthcare Revenue Cycle Management Market is evolving rapidly as providers strive to align clinical performance with robust financial outcomes. Strategic investments in digital transformation, regulatory compliance, and patient-centric payment solutions are now central to driving efficiency and sustaining competitiveness across care settings.
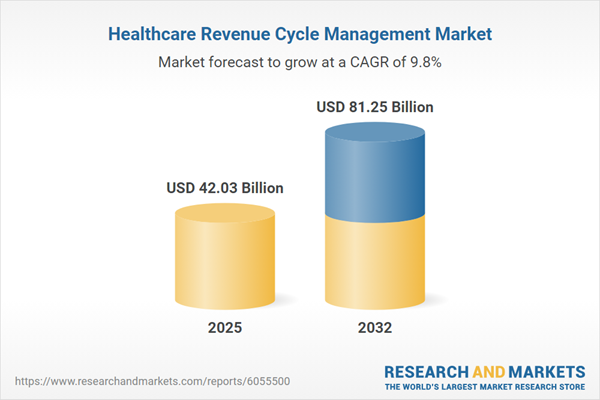
Market Snapshot: Healthcare Revenue Cycle Management Market
The Healthcare Revenue Cycle Management Market grew from USD 38.46 billion in 2024 to USD 42.03 billion in 2025 and is projected to continue expanding at a CAGR of 9.79%, reaching USD 81.25 billion by 2032.
Scope & Segmentation
- Solution: Billing and Coding Services (including inpatient, outpatient, and professional coding), Claims Management, Denial Management (appeals, tracking/reporting, pre-denial prevention), Eligibility Management, Patient Payment Solutions, Revenue Integrity Management.
- Type: In-house RCM, Outsourced RCM.
- Deployment Mode: Cloud Based, On-Premise.
- End-User: Ambulatory Services, Clinics, Hospitals.
- Region: Americas (United States, Canada, Mexico, Brazil, Argentina, Chile, Colombia, Peru), Europe, Middle East & Africa (United Kingdom, Germany, France, Russia, Italy, Spain, Netherlands, Sweden, Poland, Switzerland, United Arab Emirates, Saudi Arabia, Qatar, Turkey, Israel, South Africa, Nigeria, Egypt, Kenya), Asia-Pacific (China, India, Japan, Australia, South Korea, Indonesia, Thailand, Malaysia, Singapore, Taiwan).
- Key Companies: Accenture plc, Access Healthcare, Advantum Health, Alvarez & Marsal Holdings, LLC, Ascent Health Solutions, CareBridge Solutions Inc, Cognizant Technology Solutions Corporation, Consentus, LLC, CoreHealth Partners Inc, Elevate Health Innovations Inc, FusionCare Technologies Inc, GeBBS Healthcare Solutions, Inc., MedEvolve, Inc., MediLink Global Inc, NextGen Health Systems Inc, NovaMed Systems Inc, Optum, Inc., Precision Healthcare Billing, Quantum Health, Inc., R1 RCM Inc., Synergen Health, Vanguard Medical Billing, WellPath Solutions Inc, Wipro Limited, Zenith Healthcare Solutions.
Key Takeaways for Senior Decision-Makers
- Automation and artificial intelligence are reshaping claims management, driving efficiencies in coding accuracy and denial prevention across provider organizations.
- Cloud-based deployment models offer scalability and reduce the burden of hardware-related capital investment, meeting evolving compliance and operational requirements.
- Evolving regulations, such as price transparency and patient billing mandates, require solutions that promote clear communication and operational agility.
- Outsourced revenue cycle management models are rising in popularity as providers seek to shift fixed costs and mitigate technology-driven volatility.
- Segment-specific needs—such as streamlined solutions for ambulatory services versus complex authorization workflows in hospitals—demand tailored technology and expert partnerships to optimize outcomes.
Tariff Impact: Navigating Technology Procurement Challenges
The expansion of multi-tier tariffs on imported healthcare technology in 2025 has introduced significant supply chain and procurement complexities. Increased costs for essential hardware, such as servers and diagnostic devices, are compelling organizations to reevaluate on-premise versus cloud-based RCM initiatives. These cost pressures also drive vendor consolidation and motivate providers to explore alternative sourcing or outsourcing arrangements, further intensifying the shift toward resilient, scalable cloud deployments.
Methodology & Data Sources
This report integrates primary interviews with revenue cycle executives, payer organizations, and administrators across geographies, complemented by secondary analysis from industry benchmarks, white papers, and regulatory databases. Data triangulation and expert panel validation were employed to ensure reliable and actionable insights.
Why This Report Matters
- Gain a strategic perspective on the interplay between evolving technology, compliance, and market dynamics in the Healthcare Revenue Cycle Management Market.
- Access actionable recommendations for vendor and solution selection, helping drive operational efficiency and revenue integrity across diverse care environments.
- Equip leadership teams with robust analyses to support capital planning, technology adoption, and patient engagement initiatives.
Conclusion
Healthcare revenue cycle management is entering a phase defined by digital innovation and structural change. Adapting to these shifts will empower providers to achieve operational resilience, optimize financial outcomes, and deliver enhanced patient experiences.
Table of Contents
3. Executive Summary
4. Market Overview
7. Cumulative Impact of Artificial Intelligence 2025
Companies Mentioned
The companies profiled in this Healthcare Revenue Cycle Management Market report include:- Accenture plc
- Access Healthcare
- Advantum Health
- Alvarez & Marsal Holdings, LLC
- Ascent Health Solutions
- CareBridge Solutions Inc
- Cognizant Technology Solutions Corporation
- Consentus, LLC
- CoreHealth Partners Inc
- Elevate Health Innovations Inc
- FusionCare Technologies Inc
- GeBBS Healthcare Solutions, Inc.
- MedEvolve, Inc.
- MediLink Global Inc
- NextGen Health Systems Inc
- NovaMed Systems Inc
- Optum, Inc.
- Precision Healthcare Billing
- Quantum Health, Inc.
- R1 RCM Inc.
- Synergen Health
- Vanguard Medical Billing
- WellPath Solutions Inc
- Wipro Limited
- Zenith Healthcare Solutions
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 192 |
| Published | November 2025 |
| Forecast Period | 2025 - 2032 |
| Estimated Market Value ( USD | $ 42.03 Billion |
| Forecasted Market Value ( USD | $ 81.25 Billion |
| Compound Annual Growth Rate | 9.7% |
| Regions Covered | Global |
| No. of Companies Mentioned | 26 |