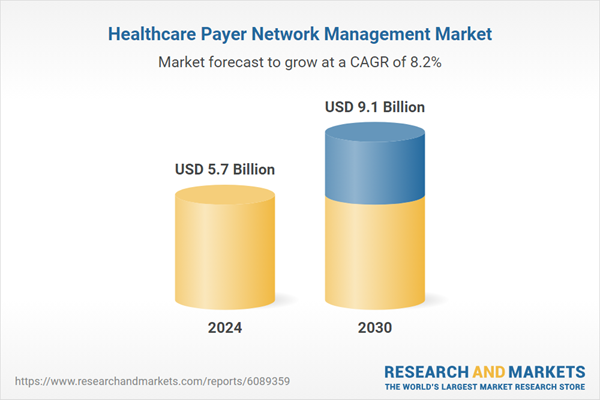
Global Healthcare Payer Network Management Market - Key Trends & Drivers Summarized
Why Is Payer Network Management Gaining Strategic Importance in Healthcare Systems?
Healthcare payer network management involves the structuring, monitoring, and optimization of provider networks by insurance companies and managed care organizations. As healthcare systems shift toward value-based care and cost containment, effective network management has become essential for delivering high-quality care while maintaining financial efficiency. A well-structured provider network enables payers to manage patient access, control service costs, and ensure adherence to clinical guidelines across in-network providers.The complexity of today's healthcare landscape - with diverse provider types, specialist tiers, and varying reimbursement contracts - has elevated network management from an administrative function to a strategic priority. Consumers are demanding more transparency, better access to care, and predictable costs, all of which depend on the quality and performance of the payer's provider network. At the same time, regulatory mandates are increasing scrutiny around network adequacy, provider directory accuracy, and patient satisfaction, compelling payers to invest in sophisticated tools and data-driven oversight mechanisms.
How Are Digital Tools and Analytics Shaping Modern Network Management?
Technological innovation is redefining how payers manage, evaluate, and optimize their provider networks. Advanced analytics platforms now enable payers to assess network adequacy, referral patterns, provider performance, and geographic coverage in real-time. AI-based tools are being used to forecast utilization trends, identify gaps in care access, and evaluate provider quality metrics such as readmission rates, patient outcomes, and cost-efficiency.Network contracting and credentialing processes are also becoming more automated, improving speed and compliance. Cloud-based solutions are helping organizations centralize provider data, improve interoperability, and facilitate continuous monitoring. Real-time directory validation and automated updates are addressing long-standing issues of outdated provider listings. These technologies not only enhance member experience but also reduce administrative overhead and regulatory penalties related to inaccurate network information.
Which Stakeholders and Regions Are Accelerating Adoption?
Health insurance companies, Medicare Advantage plans, and managed care organizations are the primary users of network management solutions, but providers themselves are becoming increasingly involved as collaborative partners in value-based arrangements. Risk-sharing contracts and bundled payment models necessitate deeper engagement between payers and providers to ensure network efficiency and performance. In large integrated delivery networks (IDNs), payer-provider partnerships are now co-developing network structures that align incentives and improve outcomes.North America remains the largest and most advanced market for healthcare payer network management due to its competitive insurance landscape and mature digital infrastructure. Europe is increasingly adopting similar models in response to cross-border healthcare needs and rising costs in public systems. In Asia-Pacific, growing private insurance markets and digitization of health administration are creating new demand for streamlined network systems, especially in countries such as India, Australia, and South Korea.
The Growth in the Healthcare Payer Network Management Market Is Driven by Several Factors
The growth in the healthcare payer network management market is driven by the transition to value-based care, the need for cost optimization, and rising regulatory scrutiny on network adequacy and transparency. Payers are increasingly relying on analytics-driven tools to build efficient, high-performing provider networks that deliver better health outcomes at lower costs. The proliferation of digital platforms, interoperability standards, and cloud-based solutions is enabling real-time visibility and agile network adjustments.Consumer demands for accessible, affordable, and transparent care are compelling payers to offer smarter, more dynamic networks. At the same time, the rise of alternative payment models is reshaping how providers are selected and evaluated, further integrating clinical and financial performance into network design. As competition intensifies and regulatory expectations increase, robust network management capabilities are becoming a core differentiator for payers seeking to balance value, quality, and growth in a rapidly evolving healthcare ecosystem.
Report Scope
The report analyzes the Healthcare Payer Network Management market, presented in terms of market value (US$). The analysis covers the key segments and geographic regions outlined below:- Segments: Solution Type (Software / Platforms, Services); Deployment (Cloud, On-Premise); End-User (Payers, Providers, Diagnostic Centers, Other End-Users).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; Spain; Russia; and Rest of Europe); Asia-Pacific (Australia; India; South Korea; and Rest of Asia-Pacific); Latin America (Argentina; Brazil; Mexico; and Rest of Latin America); Middle East (Iran; Israel; Saudi Arabia; United Arab Emirates; and Rest of Middle East); and Africa.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Software / Platforms segment, which is expected to reach US$6.8 Billion by 2030 with a CAGR of a 9.3%. The Services segment is also set to grow at 5.3% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $1.5 Billion in 2024, and China, forecasted to grow at an impressive 13% CAGR to reach $2 Billion by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Healthcare Payer Network Management Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Healthcare Payer Network Management Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Healthcare Payer Network Management Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as CGI Inc., Codoxo, Conduent Inc., Cotiviti, DXC Technology and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 42 companies featured in this Healthcare Payer Network Management market report include:
- Andros
- Appian Corporation
- Arcadia
- Athenahealth
- Availity
- Centene Corporation
- Change Healthcare
- Clarify Health
- Cognizant Technology Solutions
- EXL Service Holdings Inc.
- Gainwell Technologies
- HCentive
- HealthEdge Software
- Infosys Limited
- Inovalon
- LexisNexis Risk Solutions
- Maximus Inc.
- Mphasis Limited
- Optum Inc.
- OSP Labs
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- Andros
- Appian Corporation
- Arcadia
- Athenahealth
- Availity
- Centene Corporation
- Change Healthcare
- Clarify Health
- Cognizant Technology Solutions
- EXL Service Holdings Inc.
- Gainwell Technologies
- HCentive
- HealthEdge Software
- Infosys Limited
- Inovalon
- LexisNexis Risk Solutions
- Maximus Inc.
- Mphasis Limited
- Optum Inc.
- OSP Labs
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 372 |
| Published | February 2026 |
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 5.7 Billion |
| Forecasted Market Value ( USD | $ 9.1 Billion |
| Compound Annual Growth Rate | 8.2% |
| Regions Covered | Global |