Global Collaborative Care Model Market - Key Trends & Drivers Summarized
Why Is the Collaborative Care Model Emerging as a Critical Framework for Integrated Behavioral Health?
The Collaborative Care Model (CoCM) is gaining prominence as an evidence-based framework designed to integrate behavioral health services within primary care settings. Addressing long-standing fragmentation between mental and physical healthcare, this model promotes coordinated, patient-centered care through a team-based approach involving primary care providers, behavioral health clinicians, and psychiatric consultants. By embedding mental health services into general medical practice, CoCM enhances access, reduces stigma, and supports early intervention - particularly for conditions such as depression, anxiety, and substance use disorders.Driven by the increasing recognition of mental health as a core determinant of overall health outcomes, this model is being actively pursued by health systems, insurers, and policymakers seeking to optimize chronic disease management and improve patient satisfaction. Evidence shows that collaborative care not only enhances clinical outcomes but also delivers cost efficiencies by reducing emergency visits, hospitalizations, and specialty referrals. As a scalable and adaptable framework, CoCM is increasingly viewed as a strategic lever to improve health equity and address unmet mental health needs across diverse populations.
How Are Digital Platforms and Clinical Protocols Enhancing the Efficacy of Collaborative Care?
Technology is playing a central role in enabling the scale and effectiveness of the Collaborative Care Model. Digital platforms are being used to facilitate care coordination, manage clinical registries, and monitor patient progress through standardized assessment tools such as PHQ-9 and GAD-7. These platforms allow behavioral care managers to track caseloads, prioritize outreach, and communicate seamlessly with primary care and psychiatric consultants - streamlining workflows and ensuring accountability across multidisciplinary teams.Clinical protocols embedded within these platforms support evidence-based treatment pathways and ensure timely adjustments based on patient response. Measurement-based care - an essential component of CoCM - is increasingly being supported by patient-facing apps and telehealth tools that facilitate remote symptom tracking and virtual consultations. As demand grows for hybrid care delivery models, the integration of digital infrastructure is making it possible for collaborative care teams to serve geographically dispersed or resource-constrained populations without compromising care quality or continuity.
Which Health Systems and Patient Populations Are Driving Adoption of the Collaborative Care Model?
Large health systems, federally qualified health centers (FQHCs), accountable care organizations (ACOs), and integrated delivery networks (IDNs) are among the most active adopters of the Collaborative Care Model. These organizations benefit from the model's alignment with value-based care goals and its ability to enhance performance metrics related to population health, care coordination, and patient satisfaction. CoCM is particularly impactful in primary care clinics where mental health resources are limited, enabling providers to offer structured psychiatric care without requiring direct psychiatrist availability onsite.Patient populations with chronic medical comorbidities - such as diabetes, cardiovascular disease, and chronic pain - are prime beneficiaries of CoCM, given the frequent overlap with behavioral health conditions. The model is also well-suited for underserved communities where barriers to mental health access are high, including rural areas, Medicaid populations, and socioeconomically disadvantaged groups. By embedding behavioral services in trusted medical environments, the model improves uptake, reduces treatment delays, and enhances adherence among patients who might otherwise avoid or disengage from standalone mental health services.
How Are Policy Support, Reimbursement Structures, and Workforce Models Influencing Scalability?
Policy backing has been instrumental in driving the expansion of collaborative care, particularly in the U.S. where the Centers for Medicare & Medicaid Services (CMS) has approved specific billing codes to reimburse CoCM services. These codes incentivize care coordination and team-based interventions, providing a viable financial model for integrating behavioral health into primary care. Commercial payers are also beginning to align reimbursement frameworks with collaborative care principles, although variability in coverage and billing complexity remains a barrier in some regions.Workforce availability and training are critical to effective implementation. The model relies on a dedicated behavioral care manager - often a licensed clinical social worker, psychologist, or nurse - supported by psychiatric consultation and primary care leadership. Expanding this workforce requires investment in cross-disciplinary training programs, clinical supervision structures, and technology adoption. Health systems that can cultivate collaborative culture and align financial incentives across care teams are more likely to sustain and scale the model successfully across diverse practice settings.
What Are the Factors Driving Growth in the Collaborative Care Model Market?
Growth in the Collaborative Care Model market is being propelled by rising awareness of the mental health crisis, the shift toward integrated and value-based healthcare, and the proven clinical and economic benefits of coordinated behavioral care. As health systems seek scalable, evidence-backed solutions to address psychiatric comorbidities within chronic disease populations, CoCM offers a structured yet flexible framework that improves outcomes while optimizing resource use. The convergence of clinical demand, policy momentum, and digital enablement is expanding adoption across public and private sectors.The sustainability of this momentum will depend on the ability of stakeholders to align reimbursement policies, build interdisciplinary capacity, and invest in digital tools that support measurement-based care at scale. As behavioral health becomes a central pillar of whole-person care, the question is whether collaborative care models can continue to evolve to meet growing complexity - delivering personalized, equitable, and cost-efficient services across diverse geographies, patient needs, and care delivery environments.
Report Scope
The report analyzes the Collaborative Care Model market, presented in terms of market value (US$). The analysis covers the key segments and geographic regions outlined below:- Segments: Deployment (Web-based, Cloud-based, On-Premise); Application (Population-based Care, Patient-centered Team Care, Measurement-based Treatment, Evidence-based Care, Accountable Care, Other Applications); End-User (Hospitals & Clinics, Ambulatory Care Centers, Rehabilitation Centers, Academic & Research Institute, Other End-Users).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; and Rest of Europe); Asia-Pacific; Rest of World.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Web-based Deployment segment, which is expected to reach US$3 Billion by 2030 with a CAGR of a 18.6%. The Cloud-based Deployment segment is also set to grow at 16.2% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $483.3 Million in 2024, and China, forecasted to grow at an impressive 16.5% CAGR to reach $745.4 Million by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Collaborative Care Model Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Collaborative Care Model Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Collaborative Care Model Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as Abbott Laboratories, AbbVie Inc., Amgen Inc., Aurobindo Pharma Ltd., Bausch Health Companies Inc. and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 48 companies featured in this Collaborative Care Model market report include:
- AIMS Center, University of Washington
- Allied Behavioral Health Integration
- Altruix
- American Psychiatric Association
- CenterWell (Humana)
- Cityblock Health
- Concert Health
- FOLX Health
- Healthy Minds Policy Initiative
- Innerworld
- Magellan Healthcare
- Manatt Health
- Mindoula Health
- Mirah
- NeuroFlow
- Pearl Health
- Primary Care Collaborative
- SAMHSA
- The Banyan
- Well Health Inc.
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- AIMS Center, University of Washington
- Allied Behavioral Health Integration
- Altruix
- American Psychiatric Association
- CenterWell (Humana)
- Cityblock Health
- Concert Health
- FOLX Health
- Healthy Minds Policy Initiative
- Innerworld
- Magellan Healthcare
- Manatt Health
- Mindoula Health
- Mirah
- NeuroFlow
- Pearl Health
- Primary Care Collaborative
- SAMHSA
- The Banyan
- Well Health Inc.
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 190 |
| Published | January 2026 |
| Forecast Period | 2024 - 2030 |
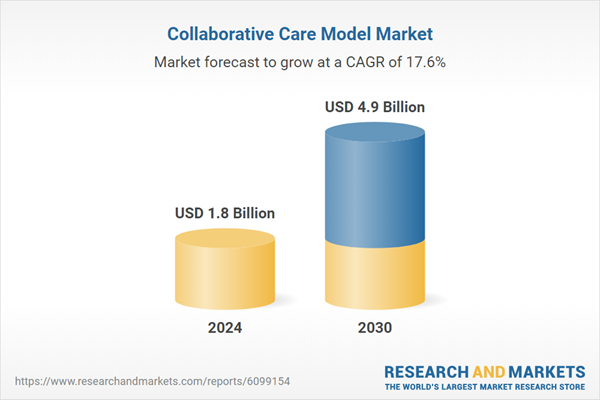
| Estimated Market Value ( USD | $ 1.8 Billion |
| Forecasted Market Value ( USD | $ 4.9 Billion |
| Compound Annual Growth Rate | 17.6% |
| Regions Covered | Global |