Speak directly to the analyst to clarify any post sales queries you may have.
10% Free customizationThis report comes with 10% free customization, enabling you to add data that meets your specific business needs.
The adoption of advanced technologies such as artificial intelligence, machine learning, and predictive analytics is further supporting market growth. These tools enable more precise decision-making and automate repetitive functions, significantly improving operational efficiency. Additionally, regulatory efforts promoting data interoperability are encouraging integration of UM platforms with electronic health records (EHRs) and clinical support systems, which in turn enhances data access and compliance. As healthcare organizations seek scalable, intelligent solutions to manage chronic conditions and improve outcomes, the demand for UM platforms is expected to increase substantially.
Key Market Drivers
Growing Emphasis on Value-Based Care and Outcome-Driven Models
A significant driver for the United States Utilization Management (UM) Solutions Market is the healthcare industry’s shift from fee-for-service to value-based care models. This transition places a strong emphasis on clinical outcomes, cost efficiency, and coordinated care delivery. UM solutions are increasingly essential in these models, ensuring that treatments adhere to evidence-based protocols and payer agreements that reward quality over quantity.The Centers for Medicare & Medicaid Services (CMS) reports that as of January 2025, over 53.4% of Traditional Medicare beneficiaries - more than 14.8 million individuals - are enrolled in accountable care arrangements aimed at enhancing care value while controlling costs. This transition underscores the vital role of UM solutions in supporting providers and payers navigating these evolving reimbursement landscapes.
Key Market Challenges
Interoperability Issues and Fragmented Health IT Infrastructure
A major challenge in the United States Utilization Management Solutions Market is the fragmented health IT ecosystem, marked by inconsistent interoperability across platforms. Providers and payers operate within disparate systems, including EHRs, payer databases, and clinical decision tools, often without standardized protocols for data exchange. This disconnect hampers seamless UM integration, delays decision-making processes, and increases administrative burden.Providers frequently face challenges aligning UM workflows with their existing health IT infrastructure, limiting access to real-time patient data and reducing visibility into the full scope of clinical information. Likewise, payers struggle to coordinate authorization workflows and claims reviews due to incompatible systems. Smaller healthcare organizations, lacking robust IT resources, are particularly disadvantaged. The inconsistent adoption of interoperability standards such as HL7 and FHIR exacerbates these issues, hindering the full realization of efficient and integrated UM operations.
Key Market Trends
Shift Toward Automation and AI-Driven Decision Support
A leading trend in the United States Utilization Management (UM) Solutions Market is the rapid shift toward AI-powered automation and decision support. Traditional UM processes are often resource-intensive and slow, creating inefficiencies in authorization and claims review procedures. AI and machine learning technologies are transforming this dynamic by automating repetitive tasks and supporting faster, more accurate decision-making.Advanced UM platforms now incorporate real-time analytics and evidence-based guidelines to assess treatment appropriateness, optimize care delivery, and reduce delays. Predictive analytics can identify at-risk patients, allowing early interventions that improve care outcomes and reduce hospitalization. Natural language processing (NLP) is being used to analyze unstructured clinical data, enhancing speed and precision in utilization review. By streamlining approvals, reducing manual workload, and improving payer-provider coordination, these AI-driven platforms are reshaping the UM landscape for enhanced efficiency and patient care.
Key Market Players
- Optum, Inc.
- Conduent, Inc.
- ZeOmega, Inc.
- HealthEdge Software, Inc.
- Keystone Peer Review Organization, LLC
- ExlService Holdings, Inc.
- Access Healthcare
- AssureCare LLC
- PrimEra Medical Technologies
- eClinicalWorks, LLC
Report Scope:
In this report, the United States Utilization Management Solutions Market has been segmented into the following categories, in addition to the industry trends which have also been detailed below:United States Utilization Management Solutions Market, By Type:
- Standalone Solutions
- Integrated Solutions
United States Utilization Management Solutions Market, By Component:
- Software Solutions
- Services
United States Utilization Management Solutions Market, By Mode of Delivery:
- Web/Cloud-Based
- On-Premise
United States Utilization Management Solutions Market, By End User:
- Healthcare Providers
- Healthcare Payers
- Others
United States Utilization Management Solutions Market, By Region:
- North-East
- Mid-West
- West
- South
Competitive Landscape
Company Profiles: Detailed analysis of the major companies present in the United States Utilization Management Solutions Market.Available Customizations:
With the given market data, the publisher offers customizations according to a company's specific needs. The following customization options are available for the report.Company Information
- Detailed analysis and profiling of additional market players (up to five).
This product will be delivered within 1-3 business days.
Table of Contents
Companies Mentioned
- Optum, Inc.
- Conduent, Inc.
- ZeOmega, Inc.
- HealthEdge Software, Inc.
- Keystone Peer Review Organization, LLC
- ExlService Holdings, Inc.
- Access Healthcare
- AssureCare LLC
- PrimEra Medical Technologies
- eClinicalWorks, LLC
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 82 |
| Published | June 2025 |
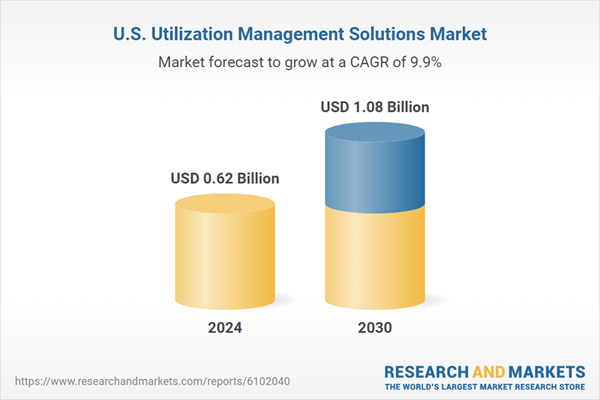
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 0.62 Billion |
| Forecasted Market Value ( USD | $ 1.08 Billion |
| Compound Annual Growth Rate | 9.8% |
| Regions Covered | United States |
| No. of Companies Mentioned | 10 |