Speak directly to the analyst to clarify any post sales queries you may have.
A clear and authoritative orientation to the evolving alcohol treatment ecosystem that frames major clinical, delivery, and commercial forces shaping decision-making
The contemporary landscape of alcohol treatment services is undergoing rapid and multifaceted change driven by advances in clinical practice, digital delivery models, shifting payer relationships, and evolving public expectations about care access and quality. This introduction frames the core themes that follow, situating operational leaders, clinicians, and purchasers in a shared context that clarifies both the immediate challenges and the strategic opportunities that lie ahead.Clinically, there is broader acceptance of integrated care that combines behavioral therapies with pharmacotherapy where appropriate, alongside an expansion of ambulatory and outpatient modalities that prioritize lower-acuity, community-based pathways. Concurrently, the role of telehealth has matured from emergency stopgap to essential modality, enabling synchronous and asynchronous engagement that complements in-person services while extending reach into underserved areas. At the same time, workforce constraints and retention pressures continue to shape service capacity, requiring active workforce development and role redesign.
From a commercial perspective, payment complexity is increasing as employer-sponsored plans, government programs, and private payers each apply distinct coverage patterns and utilization management approaches. Regulatory shifts and societal imperatives to reduce stigma are prompting new collaborations between hospitals, community clinics, and rehabilitation providers. Taken together, these dynamics create both a narrower path for program sustainability and a wider set of strategic options for organizations prepared to align clinical effectiveness with operational resilience. In short, understanding these interdependent trends is essential for leaders seeking to optimize patient outcomes while maintaining financial and organizational viability.
An in-depth exploration of how clinical innovations delivery redesign and payment evolution are reshaping provider strategy and competitive positioning
The sector’s transformative shifts are simultaneous and reinforcing, producing new care pathways and competitive configurations that require strategic recalibration. Treatment models are migrating toward greater flexibility: ambulatory services and outpatient programs are developing more robust clinical pathways that reduce reliance on inpatient beds, while residential programs are differentiating by length of stay and clinical intensity to meet diverse patient needs. Detoxification practice itself is bifurcating into ambulatory detox pathways and medically supervised inpatient detox, each with distinct clinical protocols and resource demands.Providers are reorganizing around integrated delivery, with clinics, hospitals, and rehabilitation centers coordinating care transitions more deliberately and telehealth providers embedding remote monitoring and digital therapeutics into standard workflows. Payment models are also shifting as employer-sponsored plans, government funding streams, and private insurers push for demonstrable outcomes, leading to tighter contracting and an emphasis on measurement-based care. Therapy innovation is occurring in parallel: behavioral interventions such as cognitive behavioral therapy, motivational interviewing, family and group therapies are increasingly combined with pharmacotherapy agents when clinically appropriate to tailor treatment plans to individual needs.
As a result, competitive advantage now accrues to organizations that can deliver coordinated, patient-centered care across multiple settings and payment arrangements. Those that invest in clinician training, digital infrastructure, and payer engagement are better positioned to respond to rising expectations for quality, access, and value, while also mitigating operational risk associated with capacity constraints and regulatory complexity.
A strategic analysis of how cumulative tariff actions in 2025 could influence procurement clinical supply chains and financial resilience across treatment services
The policy environment and trade dynamics can exert indirect but meaningful effects on the operational cost structure and supply chains supporting alcohol treatment services. In particular, tariff actions affecting imported pharmaceuticals, medical supplies, and digital hardware can increase procurement complexity for providers that depend on global supply lines. This creates pressure on procurement budgets and can force clinical teams to evaluate alternative medication sourcing strategies, generic substitutions, or different equipment configurations while ensuring clinical standards are maintained.Beyond direct procurement impacts, cumulative tariff effects can influence broader market conditions by contributing to cost inflation for healthcare inputs and by altering the economics of telehealth hardware and peripheral devices used in remote monitoring. Consequently, payer negotiations and reimbursement arrangements can come under strain as providers seek to preserve margin and sustain program capacity. In response, organizations have begun to diversify supply chains, prioritize domestically sourced or locally manufactured alternatives where feasible, and deepen inventory management discipline to reduce exposure to trade shocks.
Importantly, the most resilient providers combine short-term mitigation tactics with medium-term strategic shifts: they standardize formularies to reduce variability, accelerate adoption of digital solutions that lower per-visit costs, and engage payers proactively to align reimbursement with evolving care models. While trade policy introduces uncertainty, it also underscores the imperative for robust operational agility and cross-functional planning that links procurement, clinical quality, and financial stewardship.
Granular segmentation insights that clarify differentiated clinical pathways payer interactions and operational priorities across treatment modalities service providers payment types therapy approaches and end users
Segmentation reveals differentiated operational and clinical imperatives that demand tailored service design and commercial approaches across treatment type, service provider type, payment mode, therapy type, and end user. When the market is disaggregated by treatment type-Ambulatory Services, Detoxification Services, Inpatient, Outpatient, and Residential Services-the lines between settings blur as ambulatory detox and medically supervised detox establish distinct care pathways, while outpatient options like day treatment and intensive outpatient programs create intermediate-intensity alternatives. Residential services split into long-term and short-term residential models, each with divergent staffing, facility, and aftercare needs.Service provider type further stratifies opportunity and capability: clinics ranging from community-based centers to specialized clinics serve local access needs, hospitals including general and psychiatric institutions integrate complex medical oversight, private practice structures encompass both group and solo practitioners who offer personalized care, rehabilitation centers differentiate between luxury and standard rehab experiences, and telehealth providers operate across asynchronous and synchronous modalities that expand reach and convenience. Payment mode exerts a powerful shaping influence-employer-sponsored insurance with employee assistance programs and employer health plans, government funding through Medicaid and Medicare, private insurance across EPO HMO and PPO arrangements, and self-pay structures from out-of-pocket to sliding-scale models each create distinct authorization, coverage, and pricing dynamics that affect utilization and revenue cycles.
Therapy type segmentation identifies clinical differentiation: behavioral therapies such as cognitive behavioral therapy, family therapy, group therapy, and motivational interviewing remain core to engagement and relapse prevention, while pharmacotherapy options like acamprosate, disulfiram, and naltrexone complement behavioral strategies and require careful medication management and adherence supports. End-user segmentation highlights demographic nuances: adolescents encompass early and late adolescent subgroups with unique developmental considerations, adults divide into young, middle-aged, and older adult cohorts with varying comorbidities and social determinants, and seniors include young and older senior segments that demand geriatric-informed care planning and coordination with chronic disease management. Together, these segmentation lenses illuminate where clinical protocols, staffing models, payer negotiations, and marketing approaches must be tailored to align capacity with patient needs and payer requirements.
Critical regional distinctions in financing delivery and cultural context that determine access pathways service design and adoption rates across global markets
Regional context matters deeply to how alcohol treatment services are organized, financed, and delivered, with distinct differences across the Americas, Europe Middle East & Africa, and Asia-Pacific regions. In the Americas, fragmented payer landscapes and a strong presence of employer-sponsored coverage coexist with government-funded programs, creating a mosaic of access pathways that favor hybrid models combining clinic-, hospital-, and community-based services. Telehealth adoption accelerated rapidly and now supports a broad array of synchronous and asynchronous engagements, though rural and underserved communities continue to experience geographic gaps in provider density.In Europe Middle East & Africa, national health systems and varying regulatory frameworks emphasize public financing and standardized pathways in many jurisdictions, while private markets and out-of-pocket models persist in others. This mix shapes the role of rehabilitation centers and private clinics, and it often incentivizes integrated pathways that leverage both hospital-based and community-based resources. Cultural attitudes and stigma around substance use also vary considerably, influencing treatment-seeking behavior and the degree to which family- and community-oriented therapies are prioritized.
Asia-Pacific presents a heterogeneous landscape where rapid urbanization and technological diffusion enable innovative digital delivery models, yet access disparities remain between metropolitan centers and remote regions. Government policies and coverage mechanisms differ widely, influencing how pharmacotherapy, inpatient care, and residential programs are paid for and regulated. Across all regions, cross-border collaboration on clinical best practices and telehealth interoperability is increasing, and providers that tailor service models to regional payer structures and cultural expectations gain a measurable advantage in both access and patient engagement.
Practical corporate-level observations on consolidation specialization digital expansion and payer alignment that define competitive advantage in treatment services
Leading organizations in the alcohol treatment ecosystem are pursuing several parallel strategies to maintain relevance and scale. Consolidation through strategic partnerships and selective acquisitions enables providers to assemble comprehensive care pathways that span ambulatory services, detox, outpatient day programs, and residential care, thereby smoothing transitions and reducing fragmentation. At the same time, specialized clinics and private practices emphasize niche differentiation-clinical specialization, tailored programming for specific demographic cohorts, or premium rehabilitation experiences-to capture distinct patient segments.Telehealth providers and digital health ventures continue to broaden their role, offering both asynchronous therapeutic content and synchronous clinical encounters that extend the clinic footprint without the capital intensity of brick-and-mortar expansion. Hospitals, particularly psychiatric and general hospitals, are integrating addiction services into broader behavioral health portfolios to provide medical oversight for complex cases. Rehabilitation centers differentiate by clinical intensity and amenities, while group and solo practitioners focus on personalized continuity of care that supports long-term recovery.
Across these organizational types, successful companies strengthen payer relationships, invest in measurement-based care to demonstrate clinical outcomes, and prioritize workforce development to stabilize staffing pipelines. Firms that align clinical rigor with scalable delivery platforms and robust payer engagement consistently outperform peers in terms of patient retention and operational resilience, even as competition for talent and shifting reimbursement priorities intensify.
Tactical and strategic recommendations that industry leaders can implement to improve clinical outcomes operational resilience and payer alignment across treatment services
Industry leaders should adopt a set of decisive actions to strengthen clinical outcomes, operational efficiency, and market positioning. First, optimize care portfolios by balancing ambulatory, outpatient, detox, inpatient, and residential offerings to create clear care pathways that reduce unnecessary transitions and improve retention. This includes investment in protocols that enable safe ambulatory detox where clinically appropriate and in stepped-care models that match intensity to need.Second, accelerate digital integration by deploying both synchronous telehealth and asynchronous engagement tools to extend reach and improve adherence, while ensuring these technologies are embedded into clinical workflows and quality measurement systems. Third, pursue payer partnerships that align incentives around outcomes rather than volume, and proactively negotiate coverage terms that reflect the value of integrated behavioral and pharmacotherapy approaches. Fourth, prioritize workforce strategies including training, alternative credentialing pathways, and role redesign to leverage peer support and allied health professionals in ways that preserve clinical quality while expanding capacity.
Finally, strengthen supply chain resilience and procurement planning to mitigate exposure to trade-related and market disruptions, and cultivate community partnerships to address social determinants of health that affect treatment engagement. Executing these actions in concert-rather than in isolation-will produce compounding benefits: improved clinical outcomes, greater operational efficiency, enhanced payer relationships, and a stronger competitive position in a rapidly evolving market.
A rigorous mixed-methods research framework combining stakeholder interviews literature synthesis claims analysis and validation workshops to ensure actionable and credible insights
The research approach underpinning this analysis integrated qualitative and quantitative techniques to develop a robust, triangulated view of the alcohol treatment landscape. Primary stakeholder interviews with clinicians, operations leaders, payer representatives, and service users provided grounded perspectives on care delivery challenges and emergent best practices. These qualitative insights were complemented by systematic reviews of clinical guidelines, peer-reviewed literature, and policy documents to ensure alignment with prevailing standards of care and regulatory expectations.Operational analysis incorporated claims and utilization pattern reviews where available, paired with facility-level case studies that illustrated practical implementation of ambulatory detox, intensive outpatient programs, and residential care models. Segmentation mapping was applied to treatment modalities, provider types, payment modes, therapy approaches, and end-user cohorts to surface differentiated needs and operational implications. Findings were validated through cross-stakeholder workshops that tested hypotheses and refined recommendations, ensuring the final conclusions reflect both empirical evidence and practitioner experience.
Ethical standards and confidentiality protocols guided all primary research activities, and methodological limitations were transparently documented to aid interpretation. This mixed-methods approach yields actionable intelligence that balances clinical rigor with real-world operational nuance, enabling decision-makers to apply insights with confidence across strategic planning, program design, and payer negotiation contexts.
A concise synthesis of the report s most consequential findings that highlights strategic priorities for organizations seeking clinical excellence and financial sustainability
The accumulated evidence points to an alcohol treatment landscape defined by integration, adaptability, and a premium on demonstrable outcomes. Clinical innovation-particularly the combination of behavioral therapies with pharmacotherapy-and delivery flexibility that leverages ambulatory, outpatient, and telehealth modalities are reshaping patient journeys. Payment complexity and regulatory variability present persistent challenges, yet they also motivate closer collaboration between providers and payers and an increased focus on measurement-based approaches that link care to meaningful outcomes.Operationally, organizations that reconfigure care pathways to reduce fragmentation, invest in workforce development, and deploy scalable digital solutions will be best positioned to respond to shifting demand and policy environments. Regionally informed strategies that respect local payer architectures and cultural expectations are likewise essential for scalable expansion. In sum, the opportunity for leaders is to translate clinical best practices into replicable, efficient service models that align with payer priorities and patient preferences, thereby delivering both improved outcomes and sustainable operations.
Moving forward, timely action on strategic priorities-service mix optimization, digital integration, payer alignment, and workforce resilience-will determine which organizations lead the transition to higher-value, more accessible alcohol treatment services. The implications are both clinical and commercial: those who act decisively will improve patient care while securing a durable competitive position in a dynamic sector.
Table of Contents
18. ResearchStatistics
19. ResearchContacts
20. ResearchArticles
21. Appendix
Companies Mentioned
- AGCO Corporation
- AgJunction Inc.
- Agworld Pty Ltd
- aWhere Inc.
- BASF SE
- Bayer AG
- CNH Industrial N.V.
- Conservis Corporation
- CropX Inc.
- Deere & Company
- DTN, LLC
- Farmers Edge Inc.
- Granular, Inc.
- IBM Corporation
- Iteris, Inc.
- Microsoft Corporation
- Oracle Corporation
- Raven Industries, Inc.
- SAP SE
- Syngenta Group
- Taranis Visual Ltd.
- The Climate Corporation
- Trimble Inc.
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 199 |
| Published | January 2026 |
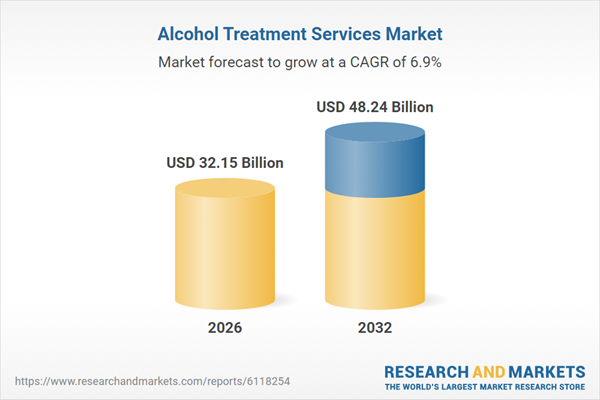
| Forecast Period | 2026 - 2032 |
| Estimated Market Value ( USD | $ 32.15 Billion |
| Forecasted Market Value ( USD | $ 48.24 Billion |
| Compound Annual Growth Rate | 6.8% |
| Regions Covered | Global |
| No. of Companies Mentioned | 23 |