Data Monetization Solutions For Healthcare Payers Market
The Data Monetization Solutions for Healthcare Payers market spans platforms and services that transform claims, eligibility, utilization, care management, provider contracting, and member engagement data into sellable or shareable assets, analytics products, and outcomes-based partnerships. Offerings include privacy-preserving data platforms, tokenization and de-identification pipelines, data marketplaces/exchanges, synthetic data generators, risk and SDOH enrichment, and API-led productization for pharma, medtech, providers, reinsurers, and employers. Recent momentum is driven by value-based care reporting, specialty drug economics, real-world evidence needs, prior-auth modernization, and AI models hungry for longitudinal, adjudicated datasets. Buyers prioritize defensible privacy engineering (HIPAA de-identification, differential privacy), robust data governance, lineage/consent management, and revenue-sharing constructs that avoid “data exhaust” leakage. Differentiation hinges on network effects (payer + provider + lab + pharmacy), standardization to modern schemas, low-latency pipelines, and pre-built use cases (adherence insights, risk adjustment, referral steering, benefit design). Go-to-market models blend direct data licensing, outcome-linked collaborations, and white-label analytics. Procurement favors platforms that co-exist with legacy cores, expose clean product catalogs (cohorts, features, RWE packs), and include audit-ready controls. As regulators and the public demand higher privacy assurance and transparency, winning programs pair rigorous governance with clear value narratives - better therapy access, fewer denials, and improved member experience - translating payer data assets into repeatable, compliant revenue.Data Monetization Solutions For Healthcare Payers Market Key Insights
- Governance-first monetization
- From raw feeds to product catalogs
- De-identification that holds analytic value
- Network effects win deals
- Outcomes-linked commercial models
- AI enablement as a pull factor
- Operational interoperability is non-negotiable
- Regulatory resilience as a differentiator
- Value stories beyond pharma
- Change management inside the payer
Data Monetization Solutions For Healthcare Payers Market Reginal Analysis
North America
Mature demand across commercial, Medicare/Medicaid plans, and PBMs fuels robust data exchanges and payer-owned marketplaces. Emphasis on HIPAA de-identification, consent provenance, and FHIR-based interoperability enables outcome-linked collaborations with pharma and providers. Buyers expect pre-built analytics (adherence, prior auth optimization), transparent data dictionaries, and strict partner vetting; large systems prize low-latency refresh and audit-ready controls.Europe
Strong data protection norms shape conservative, consortium-led models with clear public interest framing (outcomes research, health system efficiency). Vendors win with privacy engineering (pseudonymization at source, differential privacy), multi-country semantic harmonization, and hospital-payer data collaboratives. Value cases center on population health, therapy access, and trial feasibility, with rigorous governance and transparent member communication.Asia-Pacific
Heterogeneous payer landscapes drive varied plays: private insurers and government schemes explore data products for fraud analytics, benefit design, and digital health partnerships. Localization, multilingual coding harmonization, and scalable tokenization are critical. Fast-growing pharma RWE demand and digital front-door ecosystems (telehealth, pharmacy e-commerce) create appetite for governed linkage of claims, labs, and wearables.Middle East & Africa
Emerging national insurance programs and private payers prioritize fraud/waste/abuse analytics, benefit optimization, and provider performance benchmarking. Greenfield architectures enable modern privacy stacks and cloud-native exchanges. Success depends on local data residency, strong consent frameworks, and turnkey dashboards that demonstrate rapid ROI for regulators and investors.South & Central America
Mixed public-private systems adopt monetization cautiously, focusing on cost containment and access equity. Opportunities cluster around specialty drug pathways, referral steering, and employer analytics. Vendors that deliver standardized cohorts, robust de-identification, and clear opt-out processes gain trust; regional hosting and bilingual data catalogs ease procurement and regulatory review.Data Monetization Solutions For Healthcare Payers Market Segmentation
By Type
- Direct Data Monetization
- Indirect Data Monetization
By Deployment Mode
- On-Premises
- Cloud
By Facility Size
- Small and Medium Facilities
- Large Facilities
Key Market players
Optum, Change Healthcare, Inovalon, Cotiviti, LexisNexis Risk Solutions, Experian Health, Datavant, HealthVerity, Komodo Health, Clarify Health, SAS, Oracle Health, Microsoft, Google Cloud, Amazon Web Services, Snowflake, MedeAnalytics, Edifecs, Arcadia, MerativeData Monetization Solutions For Healthcare Payers Market Analytics
The report employs rigorous tools, including Porter’s Five Forces, value chain mapping, and scenario-based modelling, to assess supply-demand dynamics. Cross-sector influences from parent, derived, and substitute markets are evaluated to identify risks and opportunities. Trade and pricing analytics provide an up-to-date view of international flows, including leading exporters, importers, and regional price trends.Macroeconomic indicators, policy frameworks such as carbon pricing and energy security strategies, and evolving consumer behaviour are considered in forecasting scenarios. Recent deal flows, partnerships, and technology innovations are incorporated to assess their impact on future market performance.
Data Monetization Solutions For Healthcare Payers Market Competitive Intelligence
The competitive landscape is mapped through proprietary frameworks, profiling leading companies with details on business models, product portfolios, financial performance, and strategic initiatives. Key developments such as mergers & acquisitions, technology collaborations, investment inflows, and regional expansions are analyzed for their competitive impact. The report also identifies emerging players and innovative startups contributing to market disruption.Regional insights highlight the most promising investment destinations, regulatory landscapes, and evolving partnerships across energy and industrial corridors.
Countries Covered
- North America - Data Monetization Solutions For Healthcare Payers market data and outlook to 2034
- United States
- Canada
- Mexico
- Europe - Data Monetization Solutions For Healthcare Payers market data and outlook to 2034
- Germany
- United Kingdom
- France
- Italy
- Spain
- BeNeLux
- Russia
- Sweden
- Asia-Pacific - Data Monetization Solutions For Healthcare Payers market data and outlook to 2034
- China
- Japan
- India
- South Korea
- Australia
- Indonesia
- Malaysia
- Vietnam
- Middle East and Africa - Data Monetization Solutions For Healthcare Payers market data and outlook to 2034
- Saudi Arabia
- South Africa
- Iran
- UAE
- Egypt
- South and Central America - Data Monetization Solutions For Healthcare Payers market data and outlook to 2034
- Brazil
- Argentina
- Chile
- Peru
Research Methodology
This study combines primary inputs from industry experts across the Data Monetization Solutions For Healthcare Payers value chain with secondary data from associations, government publications, trade databases, and company disclosures. Proprietary modeling techniques, including data triangulation, statistical correlation, and scenario planning, are applied to deliver reliable market sizing and forecasting.Key Questions Addressed
- What is the current and forecast market size of the Data Monetization Solutions For Healthcare Payers industry at global, regional, and country levels?
- Which types, applications, and technologies present the highest growth potential?
- How are supply chains adapting to geopolitical and economic shocks?
- What role do policy frameworks, trade flows, and sustainability targets play in shaping demand?
- Who are the leading players, and how are their strategies evolving in the face of global uncertainty?
- Which regional “hotspots” and customer segments will outpace the market, and what go-to-market and partnership models best support entry and expansion?
- Where are the most investable opportunities - across technology roadmaps, sustainability-linked innovation, and M&A - and what is the best segment to invest over the next 3-5 years?
Your Key Takeaways from the Data Monetization Solutions For Healthcare Payers Market Report
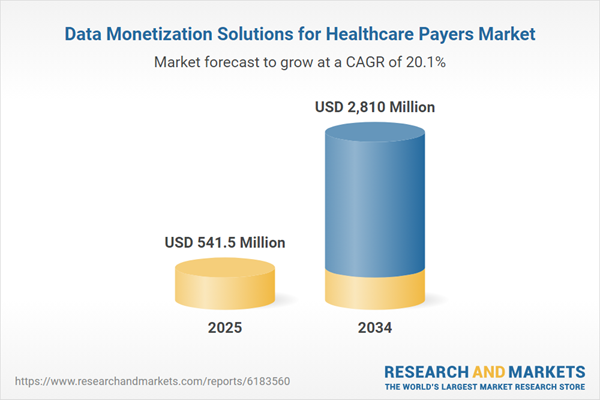
- Global Data Monetization Solutions For Healthcare Payers market size and growth projections (CAGR), 2024-2034
- Impact of Russia-Ukraine, Israel-Palestine, and Hamas conflicts on Data Monetization Solutions For Healthcare Payers trade, costs, and supply chains
- Data Monetization Solutions For Healthcare Payers market size, share, and outlook across 5 regions and 27 countries, 2023-2034
- Data Monetization Solutions For Healthcare Payers market size, CAGR, and market share of key products, applications, and end-user verticals, 2023-2034
- Short- and long-term Data Monetization Solutions For Healthcare Payers market trends, drivers, restraints, and opportunities
- Porter’s Five Forces analysis, technological developments, and Data Monetization Solutions For Healthcare Payers supply chain analysis
- Data Monetization Solutions For Healthcare Payers trade analysis, Data Monetization Solutions For Healthcare Payers market price analysis, and Data Monetization Solutions For Healthcare Payers supply/demand dynamics
- Profiles of 5 leading companies - overview, key strategies, financials, and products
- Latest Data Monetization Solutions For Healthcare Payers market news and developments
Additional Support
With the purchase of this report, you will receive:- An updated PDF report and an MS Excel data workbook containing all market tables and figures for easy analysis.
- 7-day post-sale analyst support for clarifications and in-scope supplementary data, ensuring the deliverable aligns precisely with your requirements.
- Complimentary report update to incorporate the latest available data and the impact of recent market developments.
This product will be delivered within 1-3 business days.
Table of Contents
Companies Mentioned
- Optum
- Change Healthcare
- Inovalon
- Cotiviti
- LexisNexis Risk Solutions
- Experian Health
- Datavant
- HealthVerity
- Komodo Health
- Clarify Health
- SAS
- Oracle Health
- Microsoft
- Google Cloud
- Amazon Web Services
- Snowflake
- MedeAnalytics
- Edifecs
- Arcadia
- Merative
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 160 |
| Published | November 2025 |
| Forecast Period | 2025 - 2034 |
| Estimated Market Value ( USD | $ 541.5 Million |
| Forecasted Market Value ( USD | $ 2810 Million |
| Compound Annual Growth Rate | 20.1% |
| Regions Covered | Global |
| No. of Companies Mentioned | 20 |