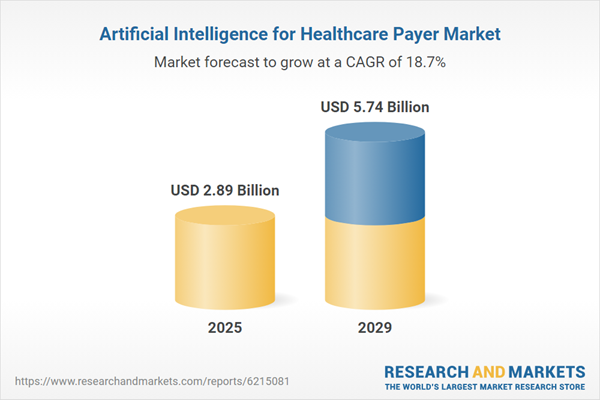
The artificial intelligence for healthcare payer market size is expected to see rapid growth in the next few years. It will grow to $5.74 billion in 2029 at a compound annual growth rate (CAGR) of 18.7%. The growth in the forecast period can be attributed to rising emphasis on value-based care models, increasing healthcare expenditure, expanding payer-provider collaborations, growing focus on member engagement and satisfaction, and rising need for real-time data insights. Key trends in the forecast period include advancements in natural language processing, development of AI-powered claim automation systems, growing research in healthcare data analytics, innovations in predictive risk modeling, emergence of explainable AI technologies, and increasing use of cloud-based AI platforms.
The growing volume of healthcare data is expected to drive the growth of artificial intelligence for the healthcare payer market going forward. Healthcare data refers to any information related to the health status, medical history, treatment, and healthcare services provided to individuals or populations. Its increasing volume is driven by digitalization, as electronic health records and connected devices enable faster and more accurate collection and analysis of patient information. Artificial intelligence (AI) for healthcare payers leverages these vast datasets from electronic health records, claims, and wearable devices to enhance decision-making through data-driven insights, enabling accurate risk assessment, fraud detection, and efficient claims management. For example, in June 2022, according to the Department of Health and Social Care, a UK-based government department, 90% of National Health Service (NHS) trusts had adopted electronic health records by December 2023 and are projected to reach 100% by March 2025. Thus, the growing volume of healthcare data is fueling the growth of artificial intelligence for the healthcare payer market.
Key companies in the artificial intelligence for healthcare payer market are focusing on developing advanced digital solutions, such as AI-powered patient navigation tools, to improve efficiency, enhance member experience, and reduce administrative burdens. AI-powered patient navigation tools are advanced digital systems that use artificial intelligence to help patients understand their benefits, find in-network care, and estimate costs. For example, in April 2024, CVS Health Corporation, a US-based health solutions company, launched a suite of new AI and digital tools. These tools include an AI-powered member experience platform designed to simplify finding in-network care and understanding costs. It features a personalized patient navigation tool that guides members to the most appropriate site of care, such as primary care, urgent care, or a specialist, based on their symptoms, benefits, and local availability, enabling seamless access to care with reduced effort.
In September 2025, Cohere Health Inc., a US-based healthcare technology company, acquired ZignaAI Inc. for an undisclosed amount. Through this acquisition, Cohere Health aims to strengthen its AI-driven payment integrity and revenue optimization capabilities, enabling health plans to automate claims validation, improve pricing accuracy, and enhance overall payer operational efficiency. ZignaAI Inc. is a US-based AI company specializing in payment integrity and revenue optimization solutions for healthcare payers.
Major companies operating in the artificial intelligence for healthcare payer market are Amazon Web Services Inc., Google LLC, Microsoft Corporation, Accenture plc., Accenture plc, Oracle Corporation, Cognizant Technology Solutions Corporation, Wipro Limited, SAS Institute Inc., Hexaware Technologies Limited, Firstsource Solutions Limited, Innovaccer Incorporated, Cohere Health Incorporated, Softheon, MST Solutions LLC, Lyric AI Incorporated, Inovaare Corporation, Codoxo, Iatros Health Incorporated, Alaffia Health Incorporated
North America was the largest region in the artificial intelligence for healthcare payer market in 2024. Asia-Pacific is expected to be the fastest-growing region in the forecast period. The regions covered in artificial intelligence for healthcare payer report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East and Africa. The countries covered in the artificial intelligence for healthcare payer market report are Australia, Brazil, China, France, Germany, India, Indonesia, Japan, Russia, South Korea, UK, USA, Canada, Italy, Spain.
Note that the outlook for this market is being affected by rapid changes in trade relations and tariffs globally. The report will be updated prior to delivery to reflect the latest status, including revised forecasts and quantified impact analysis. The report’s Recommendations and Conclusions sections will be updated to give strategies for entities dealing with the fast-moving international environment.
The sudden escalation of U.S. tariffs and the consequent trade frictions in spring 2025 are severely impacting the healthcare sector, particularly in the supply of critical medical devices, diagnostic equipment, and pharmaceuticals. Hospitals and healthcare providers are facing higher costs for imported surgical instruments, imaging equipment, and consumables such as syringes and catheters, many of which have limited domestic alternatives. These increased costs are straining healthcare budgets, leading some providers to delay equipment upgrades or pass on expenses to patients. Additionally, tariffs on raw materials and components are disrupting the production of essential drugs and devices, causing supply chain bottlenecks. In response, the industry is diversifying sourcing strategies, boosting local manufacturing where possible, and advocating for tariff exemptions on life-saving medical products.
The artificial intelligence for healthcare payer market research report is one of a series of new reports that provides artificial intelligence for healthcare payer market statistics, including artificial intelligence for healthcare payer industry global market size, regional shares, competitors with a artificial intelligence for healthcare payer market share, detailed artificial intelligence for healthcare payer market segments, market trends and opportunities, and any further data you may need to thrive in the artificial intelligence for healthcare payer industry. This artificial intelligence for healthcare payer market research report delivers a complete perspective of everything you need, with an in-depth analysis of the current and future scenario of the industry.
Artificial intelligence for healthcare payer refers to the use of AI technologies to optimize administrative, financial, and clinical decision-making processes within health insurance and payer organizations. Its primary purpose is to improve claims processing, detect fraud, enhance member engagement, and support cost-effective, data-driven care management.
The key components of artificial intelligence for healthcare payer are software and services. Software refers to AI-driven applications that automate claims, detect fraud, predict risks, and enhance decision-making to improve payer efficiency and cost management. It is powered by technologies such as machine learning (ML), natural language processing (NLP), and others, and is deployed through cloud and on-premises models. It finds applications in claims processing optimization, fraud detection and prevention, revenue management and billing, member engagement and personalization, risk adjustment and predictive analytics, administrative workflow automation, and others.
The artificial intelligence for healthcare payer market consists of revenues earned by entities by providing services such as data analytics, predictive modeling, patient engagement, prior authorization automation, healthcare data integration, and clinical decision support services. The market value includes the value of related goods sold by the service provider or included within the service offering. The artificial intelligence for healthcare payer also includes sales of automated claims processing systems, predictive risk modeling software, healthcare data management systems, clinical decision support tools, fraud detection devices, AI-driven chatbots, data storage servers, and workflow automation tools. Values in this market are ‘factory gate’ values, that is the value of goods sold by the manufacturers or creators of the goods, whether to other entities (including downstream manufacturers, wholesalers, distributors and retailers) or directly to end customers. The value of goods in this market includes related services sold by the creators of the goods.
The market value is defined as the revenues that enterprises gain from the sale of goods and/or services within the specified market and geography through sales, grants, or donations in terms of the currency (in USD unless otherwise specified).
The revenues for a specified geography are consumption values that are revenues generated by organizations in the specified geography within the market, irrespective of where they are produced. It does not include revenues from resales along the supply chain, either further along the supply chain or as part of other products.
This product will be delivered within 3-5 business days.
Table of Contents
Executive Summary
Artificial Intelligence for Healthcare Payer Global Market Report 2025 provides strategists, marketers and senior management with the critical information they need to assess the market.This report focuses on artificial intelligence for healthcare payer market which is experiencing strong growth. the report gives a guide to the trends which will be shaping the market over the next ten years and beyond.
Reasons to Purchase:
- Gain a truly global perspective with the most comprehensive report available on this market covering 15 geographies.
- Assess the impact of key macro factors such as geopolitical conflicts, trade policies and tariffs, post-pandemic supply chain realignment, inflation and interest rate fluctuations, and evolving regulatory landscapes.
- Create regional and country strategies on the basis of local data and analysis.
- Identify growth segments for investment.
- Outperform competitors using forecast data and the drivers and trends shaping the market.
- Understand customers based on the latest market shares.
- Benchmark performance against key competitors.
- Suitable for supporting your internal and external presentations with reliable high quality data and analysis
- Report will be updated with the latest data and delivered to you along with an Excel data sheet for easy data extraction and analysis.
- All data from the report will also be delivered in an excel dashboard format.
Description
Where is the largest and fastest growing market for artificial intelligence for healthcare payer? How does the market relate to the overall economy, demography and other similar markets? What forces will shape the market going forward, including technological disruption, regulatory shifts, and changing consumer preferences? The artificial intelligence for healthcare payer market global report answers all these questions and many more.The report covers market characteristics, size and growth, segmentation, regional and country breakdowns, competitive landscape, market shares, trends and strategies for this market. It traces the market’s historic and forecast market growth by geography.
- The market characteristics section of the report defines and explains the market.
- The market size section gives the market size ($b) covering both the historic growth of the market, and forecasting its development.
- The forecasts are made after considering the major factors currently impacting the market. These include: the technological advancements such as AI and automation, Russia-Ukraine war, trade tariffs (government-imposed import/export duties), elevated inflation and interest rates.
- Market segmentations break down the market into sub markets.
- The regional and country breakdowns section gives an analysis of the market in each geography and the size of the market by geography and compares their historic and forecast growth.
- The competitive landscape chapter gives a description of the competitive nature of the market, market shares, and a description of the leading companies. Key financial deals which have shaped the market in recent years are identified.
- The trends and strategies section analyses the shape of the market as it emerges from the crisis and suggests how companies can grow as the market recovers.
Report Scope
Markets Covered:
1) By Component: Software; Services2) By Technology: Machine Learning (ML); Natural Language Processing (NLP); Other Technologies
3) By Deployment: Cloud; on-Premises
4) By Application: Claims Processing Optimization; Fraud Detection and Prevention; Revenue Management and Billing; Member Engagement and Personalization; Risk Adjustment and Predictive Analytics; Administrative Workflow Automation; Other Applications
Subsegments:
1) By Software: Predictive Analytics Platforms; Claims Management Solutions; Fraud Detection Systems; Risk Assessment Tools; Member Engagement Solutions2) By Services: Implementation and Integration Services; Consulting Services; Support and Maintenance Services; Training and Education Services; Managed Services
Companies Mentioned: Amazon Web Services Inc.; Google LLC; Microsoft Corporation; Accenture plc.; Accenture plc; Oracle Corporation; Cognizant Technology Solutions Corporation; Wipro Limited; SAS Institute Inc.; Hexaware Technologies Limited; Firstsource Solutions Limited; Innovaccer Incorporated; Cohere Health Incorporated; Softheon; MST Solutions LLC; Lyric AI Incorporated; Inovaare Corporation; Codoxo; Iatros Health Incorporated; Alaffia Health Incorporated
Companies Mentioned
The companies profiled in this Artificial Intelligence for Healthcare Payer market report include:- Amazon Web Services Inc.
- Google LLC
- Microsoft Corporation
- Accenture plc.
- Accenture plc
- Oracle Corporation
- Cognizant Technology Solutions Corporation
- Wipro Limited
- SAS Institute Inc.
- Hexaware Technologies Limited
- Firstsource Solutions Limited
- Innovaccer Incorporated
- Cohere Health Incorporated
- Softheon
- MST Solutions LLC
- Lyric AI Incorporated
- Inovaare Corporation
- Codoxo
- Iatros Health Incorporated
- Alaffia Health Incorporated
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 250 |
| Published | December 2025 |
| Forecast Period | 2025 - 2029 |
| Estimated Market Value ( USD | $ 2.89 Billion |
| Forecasted Market Value ( USD | $ 5.74 Billion |
| Compound Annual Growth Rate | 18.7% |
| Regions Covered | Global |
| No. of Companies Mentioned | 21 |